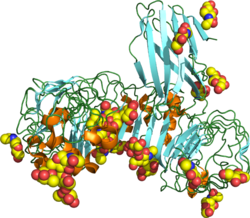
Toll-like receptor 4 (TLR4), also designated as CD284 (cluster of differentiation 284), is a key activator of the innate immune response and plays a central role in the fight against bacterial infections. TLR4 is a transmembrane protein of approximately 95 kDa that is encoded by the TLR4 gene.
TLR4 belongs to the toll-like receptor family which is representative of the pattern recognition receptors (PRR), so named for their ability to recognize evolutionarily conserved components of microorganisms (bacteria, viruses, fungi and parasites) called pathogen-associated molecular patterns (PAMPs). The recognition of a PAMP by a PRR triggers rapid activation of the innate immunity essential to fight infectious diseases.[5]
TLR4 is expressed in immune cells mainly of myeloid origin, including monocytes, macrophages and dendritic cells (DC).[5] It is also expressed at a lower level on some non-immune cells, including epithelium, endothelium, placental cells and beta cells in Langerhans islets. Most myeloid cells express also high amounts of plasma membrane-anchored CD14, which facilitates the activation of TLR4 by LPS and controls the subsequent internalization of the LPS-activated TLR4 important for receptor signaling and degradation.[6][7]
The main ligands for TLR4 are lipopolysaccharides (LPS), the major components of the outer membrane of Gram-negative bacteria and some Gram-positive bacteria. TLR4 can also be activated by endogenous compounds called damage-associated molecular patterns (DAMPs), including high mobility group box protein 1 (HMGB1), S100 proteins, or histones. These compounds are released during tissue injury and by dying or necrotic cells.[8][9][10][11][12]
Function
editThe first function described for TLR4 was the recognition of exogenous molecules from pathogens (PAMPs), in particular LPS molecules from gram-negative bacteria.[13] As pattern recognition receptor, TLR4 plays a fundamental role in pathogen recognition and activation of innate immunity which is the first line of defense against invading micro-organisms. During infection, TLR4 responds to the LPS present in tissues and the bloodstream and triggers pro-inflammatory reactions facilitating eradication of the invading bacteria.[13]
TLR4 is also involved in the recognition of endogenous DAMP molecules leading to different signaling outcomes than PAMPs, both quantitatively and qualitatively.[14][12] DAMPs can activate TLR4 in non-infectious conditions to induce tissue repair and the activation of mainly proinflammatory responses.[8][9][10][11][12] Generally, inflammation has a protective role. It is a complex and coordinated process followed by the induction of resolution pathways that restore tissue integrity and function. However, in some cases, an excessive and/or poorly regulated inflammatory response to DAMPs can be detrimental to the organism, accelerating the development or progression of pathologies such as a number of cancers and neurodegenerative diseases (as discussed below).
TLR4 binds LPS with the help of LPS-binding protein (LBP) and CD14, and an indispensable contribution of the MD-2 protein stably associated with the extracellular fragment of the receptor.[15] TLR4 signaling responds to signals by forming a complex using an extracellular leucine-rich repeat domain (LRR) and an intracellular toll/interleukin-1 receptor (TIR) domain. LPS stimulation induces a series of interactions with several accessory proteins which form the TLR4 complex on the cell surface. LPS recognition is initiated by an LPS binding to an LBP protein. This LPS-LBP complex transfers the LPS to CD14 which is a glycosylphosphatidylinositol-anchored membrane protein that binds the LPS-LBP complex and facilitates the transfer of LPS to MD-2 protein, which is associated with the extracellular domain of TLR4. LPS binding promotes the dimerization of TLR4/MD-2 complex. The conformational changes of the TLR4 induce the recruitment of intracellular adaptor proteins containing the TIR domain which is necessary to activate the downstream signaling pathway.
The binding of an LPS molecule to the TLR4/MD-2 complex involves acyl chains and phosphate groups of lipid A, the conserved part of LPS and the main inducer of pro-inflammatory responses to LPS.[16][17]
TLR4 activation and response to LPS is greatly influenced by the polysaccharide domain and the molecular structure of Lipid A moiety of the LPS molecules. Hexa-acylated and diphosphorylated LPS, like Escherichia coli LPS (O111:B4), is one of the most potent agonists of TLR4 whereas under-acylated LPS and dephosphorylated LPS species have a weaker pro-inflammatory activity especially in human cells.[18] Structural determinants of this phenomenon are found in the TLR4/MD-2 complex and also in CD14 protein.[16][19] The polysaccharide portion covalently bound to lipid A plays also and indispensable role in TLR4 activation through CD14/TLR4/MD-2.[20] However, in addition to the lipid A domain, the polysaccharide moiety plays an important role in the binding and activation of the LPS molecules as the lipid A moiety alone was demonstrated to be significantly less active than the full LPS molecule.[21]
Signaling
editUnlike all the other TLRs, TLR4 stimulation triggers two signaling pathways called the MyD88-dependent and the TRIF-dependent one after the adaptor proteins involved in their induction.[22] The MyD88-dependent signaling is triggered by TLR4 localized to the plasma membrane, while the TRIF-dependent one by the TLR4 internalized in endosomes.
These signaling pathways lead to the production of two sets of cytokines. The MyD88-dependent pathway induces the production of pro-inflammatory cytokines while TRIF-dependent pathway induces the production of type I interferons and chemokines.[22][23] The molecular structure of TLR4 ligands (in particular LPS), as well as their complexation with proteins or lipids, greatly influence the action of these TLR4-related signaling pathways, leading to different cytokine balances. [24][25][26][27]
MyD88 – dependent pathway
editThe MyD88-dependent pathway is regulated by two adaptor-associated proteins: Myeloid Differentiation Primary Response Gene 88 (MyD88) and TIR Domain-Containing Adaptor Protein (TIRAP). It also involves the activation of IL-1 Receptor-Associated Kinases (IRAKs) and the adaptor molecules TNF Receptor-Associated Factor 6 (TRAF6). TRAF6 induces the activation of TAK1 (Transforming growth factor-β-Activated Kinase 1) that leads to the activation of MAPK cascades (Mitogen-Activated Protein Kinase) and the IκB Kinases (IKK), called IKKα and IKKβ.[28] IKKs' signaling pathway leads to the induction of the transcription factor NF-κB, while activation of MAPK cascades lead to the activation of another transcription factor AP-1.[28][29] These two transcription factorsnduces the expression of genes encoding pro-inflammatory mediators, such as tumor necrosis factor α (TNF-α), interleukin (IL)-6, and type III interferons (IFNλ1/2).[30][31][32]
TRIF – dependent pathway
editThe TRIF-dependent pathway involves the internalization of TLR4 in endosomes and the recruitment of the adaptor proteins TIR-domain-containing adaptor inducing interferon-β (TRIF) and TRIF-related Adaptor Molecule (TRAM). TRAM-TRIF signals activate the ubiquitin ligase TRAF3 followed by the activation of non-canonical IKK kinases: TANK binding kinase 1 (TBK1) and IKKε. TBK1 phosphorylates the pLxIS consensus motif of TRIF that is necessary to recruit interferon regulatory factor (IRF) 3. IRF3 is also phosphorylated by TBK1 and then dissociates from TRIF, dimerizes and translocates to the nucleus.[33] Finally, IRF3 induces the expression of genes encoding type I IFN such as interferon beta (IFN-β), the chemokine CCL5/ RANTES and interferon-regulated genes as that encoding the chemokine CXCL10/IP-10.[30][31][32][34] TRIF-dependent signaling pathway of TLR4 is known to play a central role in the stimulation of innate immune cells such as macrophages, the maturation of DCs and the induction and recruitment of Th1 adaptive immune responses.[35]
Immune cell activation
editTLR4 activation by LPS enables a rapid stimulation of a whide range of innate immune cells such as macrophages and DCs. This leads to the secretion of pro-inflammatory and type I interferons cytokines, chemokines. Production levels of these cytokines/chemokines vary according to the degree of activation of the MyD88 and TRIF signaling pathways by TLR4 agonist molecules. TLR4 activation also induces the stimulation of antigen presentation and upregulation of costimulatory molecules (such as CD40, CD80 and CD86) on innate immune cells which are required for antigen presentation for T lymphocytes.[36][37] This explains why TLR4 activation by LPS is also known to stimulate the generation of effective adaptive immune responses and to induce their recruitment, polarization and maintenance via the panel of cytokines and chemokines produced. [37][22]
The TRIF and MyD88 signaling pathways have a different but complementary impact on immune cell activation. Macrophages stimulation has been shown to be strictly dependent on TRIF pathway activation whereas DC activation and maturation depend on both the MyD88 and TRIF pathways. [38][39][40][41] The increased expression of costimulatory and MHC molecules is a hallmark of DC maturation required for antigen presentation by these cells. [42] However, significant differences were found in the signaling pathways leading to this phenomenon. In macrophages, the upregulation of costimulatory molecules depends strictly on the TRIF-dependent pathway, whereas in DC both the MyD88- and TRIF-dependent ones are involved.[43][44][22][45] The increased cell surface presence of the costimulatory molecules and also of MHC II is a hallmark of DC maturation required for antigen presentation by these cells.[46]
The activation of MyD88 and TRIF signaling pathways were also found to induce Th1 polarization of the T cells responses through DC maturation and the panel of cytokines produced. [47][48][49] Low activation of MYD88 pathway is however important for effective cytotoxic T-cell differentiation by facilitating fusion of MHC I-bearing recycling endosomes with phagosomes allowing cross-presentation of antigens.[47] In contrast, robust activation of MYD88 pathway induces excessive production of pro-inflammatory cytokines leading to life-threatening pathological consequences such as cytokine storms.
The impact of TLR4 activation on the innate and adaptive immune system explains why TLR4 agonists, such as LPS derivatives, have been developed as vaccine adjuvants. Among them is GSK's Monophosphorylated Lipid A (MPL), a detoxified Lipid A derived from Salmonella LPS, which is the first and only natural immunostimulant to have been approved as adjuvant in five human vaccines.[50][51][52]
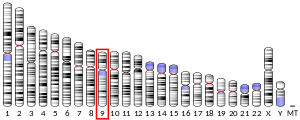
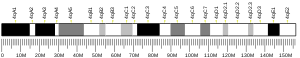
Evolutionary history and polymorphism
editTLR4 originated when TLR2 and TLR4 diverged about 500 million years ago near the beginning of vertebrate evolution.[53] Sequence alignments of human and great ape TLR4 exons have demonstrated that not much evolution has occurred in human TLR4 since our divergence from our last common ancestor with chimpanzees; human and chimp TLR4 exons only differ by three substitutions while humans and baboons are 93.5% similar in the extracellular domain.[54] Notably, humans possess a greater number of early stop codons in TLR4 than great apes; in a study of 158 humans worldwide, 0.6% had a nonsense mutation.[55][56] This suggests that there are weaker evolutionary pressures on the human TLR4 than on our primate relatives. The distribution of human TLR4 polymorphisms matches the out-of-Africa migration, and it is likely that the polymorphisms were generated in Africa before migration to other continents.[56][57]
Various single nucleotide polymorphisms (SNPs) of TLR4 have been identified in humans . For some of them, an association with increased susceptibility to Gram-negative bacterial infections or faster progression and a more severe course of sepsis in critically ill patients was reported.However, they are very rare, and their frequency varies according to ethnic origin. The 2 predominant SNPs are Asp299Gly and Thr399Ile, with a frequency of <10% in the Caucasian population and even lower in the Asian population.[58] These two SNPs are missense mutations, thus associated with a loss of function, which may explain their negative impact on infection control. Studies have indeed shown that TLR4 D299G SNP limits the response to LPS by compromising MyD88 and TRIF recruitment to TLR4, and thus cytokine secretion, but without affecting TLR4 expression [59][60] Structural analyses of human TLR4 with SNP D299G suggest that this amino acid change affects van der Waals interaction and hydrogen bonding in leucine-rich repeats, modulating its surface properties which may affect LPS ligand binding to TLR4.[61]
Clinical significance
editTLR4 has been reported to play both friend and foe in a variety of human diseases, such as bacterial infections and cancers. This dual role of TLR4 depends on the intensity, duration and site (surface or endosome) of its activation, its polymorphism and the balance of activation of signaling pathways (MyD88 vs. TRIF).
Infectious diseases
editTLR4 play a central role in the control of bacterial infections through the recognition of LPS molecules from gram-negative, and some gram-positive, bacteria.[62] During infections, TLR4s on innate immunity cells are activated by LPS molecules present in tissues and the bloodstream. This activates innate immunity, the first line of defense against invading microorganisms, and triggers pro-inflammatory responses that facilitate the eradication of invading bacteria.[13] Generally, inflammation has a protective role. It is a complex and coordinated process followed by the induction of resolution pathways that restore tissue integrity and function. However, in some cases, exaggerated and uncontrolled inflammation triggered by TLR4 during infection can lead to sepsis and septic shock.[33] Infections with Gram-negative bacteria such as Escherichia coli and Pseudomonas aeruginosa are the prevailing causes of severe sepsis in humans.Some studies have linked TLR4 polymorphisms (Asp299Gly and Thr399Ile SNPs) to an increased susceptibility to sepsis due to gram-negative infection but other studies failed to confirm this.[63]
Cancer
editThe role of the TLR4 in the control of cancer progression and in cancer therapy is well documented.
Stimulation of TLR4 by natural derivatives and LPS is well known to induce potent antitumor activity. This anti-tumor activity is linked to the ability of LPS to stimulate innate immunity via TLR4, resulting in the production of pro-inflammatory cytokines and type 1 interferons, and the indirect generation of adaptive anti-tumor responses.[64][65]
The first clues about the efficacy of TLR4 agonists like LPS in cancer immunotherapy was found in the 19th centuries, when bacterial infections were found to induce tumor regressions.[66] Later, Dr William Coley showed the therapeutic efficacy of a mixed bacterial vaccine, so-called “Coley’s toxin”, to human cancer.[67] Since then, a number of developments have been made in the treatment or prevention of cancer using bacterial mixtures strongly activating TLR4 due to LPS content. The antituberculosis vaccine Bacillus Calmette–Guérin (BCG) was approved by the Federal Drug Administration (FDA) in 1990 for the local treatment of superficial bladder cancer. BCG promotes dendritic cell maturation, and this effect is TLR4 (as well as TLR2) dependent.[68] There are also reports on the treatment of oral squamous cell carcinoma, gastric , Head-and-neck and cervical cancers with lyophilized streptococcal preparation OK-432 (Picibanil).[69] The mechanism of action of OK-432 involves TLR4 activation, since OKA-432 does not inhibit tumor growth on TLR4 knockouts as it does on wild-type mice.[70]
Purified LPS also showed potent anti-tumor efficacy as systemic therapeutic agents in several tumor models.[71][72] In the 90’s, clinical trials evaluating the intravenous administration of LPS to patients with cancer provided positive results including several cases of disease stabilization and partial responses. However, limiting toxicities at doses in the ng/kg range has been reported which are too low to obtain significant antitumor effects.[73]
Subsequently, detoxified TLR4 agonists (LPS derivatives) have been produced and evaluated in the clinic. This includes the MPL, a chemically modified LPS which was the first TLR4 agonist to be approved and commercialized by GSK in 5 human vaccines (HPV, Zoster, Hepatitis B, Malaria, RSV). MPL was investigated as an adjuvant for curative anti-tumor vaccines, with the approval of Melacine in Canada for the treatment of patients with malignant melanoma.[74] Synthetic LPS derivatives based on dephosphorylated lipid A moiety structures were also developed and confirmed potent adjuvant and antitumor activities as therapeutic agents. In particular, the intratumoral administration of Glucopyranosyl Lipid Adjuvant (GLA-SE/G100), a synthetic detoxified analog of lipid A formulated in a stable emulsion, showed anti-tumor immune responses and tumor regression in patients with Merkel cell carcinoma,[75] and potent adjuvant activity in phase 2 trials in combination with pembrolizumab in patients with follicular lymphoma.[76][77]
Besides the recognized anti-tumor efficacy of TLR4 activation by LPS, some studies suggest that TLR4 may also contribute to the development of some cancers, (prostate, liver, breast and lung cancers) and may contribute to resistance to paclitaxel chemotherapy in breast cancer.[78] Some clinical studies also suggested a potential correlation between TLR4 expression on tumor cells and tumor progression. However, no such effect was reported in the numerous clinical studies conducted with natural LPS or LPS derivatives. On the contrary, in phase 2 studies with GLA, a positive association between baseline TLR4 expression in tumors and the increase of overall response rates has been reported.[77]
The potential impact of TLR4 on the progression of some cancers was associated with the excessive production of pro-inflammatory cytokines via activation of the TLR4-MyD88/NF-kB signaling pathway.[79][80][81] Several studies showed that this is mediated by the misuse of DAMP signaling by tumor cells.[12][82][14]
Many DAMPs are released by dying or necrotic tumor cells and present during cancer progression. DAMPs released from tumor cells can directly activate tumor-expressed TLR4 that induce chemoresistance, migration, invasion, and metastasis. Furthermore, DAMP-induced chronic inflammation in the tumor microenvironment causes an increase in immunosuppressive populations, such as M2 macrophages, myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs).[12] DAMPs, such as HMGB1, S100 proteins, and heat shock proteins (HSPs), were found to strongly activate inflammatory pathways and release IL-1, IL-6, LT-β, IFN-γ, TNF, and transforming growth factor (TGF)-β promoting inflammation, immunosuppression, angiogenesis, and tumor cell proliferation.[11]
Several studies have evaluated the potential association of this TLR4 polymorphism with cancer risk, but the data are highly conflicting. However, some meta-analyses suggest an association of SNP D299G with gastric, viral-induced and female-specific cancers (cervix, ovary).[83]
Neurogenerative diseases
editGrowing evidence suggests an implication of TLR4 in the development and progression of neurogenerative disorders such as Alzheimer's disease, Parkinson's disease, and Huntington's disease. In the brain, TLR4 is expressed by neurons as well as the non-neuronal glial cells, which include microglia, astrocytes, and oligodendrocytes. TLR4 is expressed primarily by microglia, and to a lesser extent by astrocytes, oligodendrocytes, and neurons.[5] Microglia are representatives of the mononuclear phagocyte system in the brain, and TLR4 activation regulates some of their functions, such as phagocytic activity.[84][13]
Activation of microglial TLR4 has been suggested to protect against or slow the development of neurodegenerative diseases, notably by enhancing the clearance of neurotoxic proteins such as Aβ and its aggregates, thanks to increased phagocytic and autophagic activity.[85]
However, chronic TLR4 activation is believed to be associated with glia-mediated neuronal death due to excessive secretion of pro-inflammatory cytotoxins leading to neuroinflammation, a key factor in the development of many neurodegenerative diseases.[86][87] In the brain, TLR4 can be activated by various endogenous DAMPs in addition to pathology-associated proteins such as aggregates of amyloid-βpeptides (Aβ) or α-synuclein.[88] All these structures bind TLR4 and activate downstream signaling pathways in glia, inducing secretion of reactive oxygen species (ROS) and proinflammatory cytokines such as IL-1β and TNF-α, which can lead to damage and death of neurons.[86][89][90] Neuronal death is accompanied by the release of DAMPs into the extracellular space, which can then further activate TLR4, aggravating neuroinflammation.[91] In patients with Alzheimer's disease (AD), the levels of circulating DAMPs like HMGB1 and soluble RAGE, are significantly elevated, which was correlated with the levels of amyloid beta.[92] In AD patients, the serum levels of S100B are also intimately related to the severity of the disease.[93] The role of the HMGB1-TLR4 axis is very important in the pathogenesis of Parkinson's disease (PD). The serum HMGB1 and TLR4 protein levels were significantly elevated in PD patients and correlated with the PD stages.[94]
Targeting TLR4 with agonists or antagonists, or modulating its downstream signaling pathways, may have a therapeutic potential in treating neurodegenerative diseases.[95] TLR4-specific antagonists could suppress neuroinflammation by reducing overproduction of inflammatory mediators and cytotoxins by glia. However, TLR4 antagonists could have adverse CNS effects by inhibiting phagocytosis by glia, reducing protein clearance, and interfering with myelination.[96] Some studies showed that selective TLR4 agonists could be beneficial by upregulating the phagocytic activity of microglia, leading to enhanced clearance of damaged tissue and abnormal protein aggregates associated with several different CNS diseases. Repeated injections of MPL, at doses that are nonpyrogenic, were found to significantly improved AD-related pathology mice.[97] MPL led to a significant reduction in Aβ load in the brain, as well as enhanced cognitive function. MPL induced a potent phagocytic response by microglia while triggering a moderate inflammatory reaction. However, adverse effects can be caused by TLR 4 agonists inducing secretion of inflammatory mediators. Studies therefore suggested that TLR4 agonists that selectively activate the TRIF signaling pathway could be highly beneficial in the treatment of neurodegenerative disorders by increasing glial cell phagocytic activity without significantly increasing glial cytokines and cytotoxins.[96]
Drugs targeting TLR4
editTLR4 has been shown to be important for the long-term side-effects of opioid analgesic drugs. Various μ-opioid receptor ligands have been tested and found to also possess action as agonists or antagonists of TLR4, with opioid agonists such as (+)-morphine being TLR4 agonists, while opioid antagonists such as naloxone were found to be TLR4 antagonists. Activation of TLR4 leads to downstream release of inflammatory modulators including TNF-α and Interleukin-1, and constant low-level release of these modulators is thought to reduce the efficacy of opioid drug treatment with time, and be involved in both the development of tolerance to opioid analgesic drugs,[98][99] and in the emergence of side-effects such as hyperalgesia and allodynia that can become a problem following extended use of opioid drugs.[100][101] Drugs that block the action of TNF-α or IL-1β have been shown to increase the analgesic effects of opioids and reduce the development of tolerance and other side-effects,[102][103] and this has also been demonstrated with drugs that block TLR4 itself.
The response of TLR4 to opioid drugs has been found to be enantiomer-independent, so the "unnatural" enantiomers of opioid drugs such as morphine and naloxone, which lack affinity for opioid receptors, still produce the same activity at TLR4 as their "normal" enantiomers.[104][105] This means that the unnatural enantiomers of opioid antagonists, such as (+)-naloxone, can be used to block the TLR4 activity of opioid analgesic drugs, while leaving the μ-opioid receptor mediated analgesic activity unaffected.[106][105][107] This may also be the mechanism behind the beneficial effect of ultra-low dose naltrexone on opioid analgesia.[108]
Morphine causes inflammation by binding to the protein lymphocyte antigen 96, which, in turn, causes the protein to bind to Toll-like receptor 4 (TLR4).[109] The morphine-induced TLR4 activation attenuates pain suppression by opioids and enhances the development of opioid tolerance and addiction, drug abuse, and other negative side effects such as respiratory depression and hyperalgesia. Drug candidates that target TLR4 may improve opioid-based pain management therapies.[110]
Agonists
editApart from LPS and its derivatives, up to 30 natural TLR4 agonists with diverse chemical structures have been postulated. However, besides DAMPs, the others have not demonstrated to be direct activators of TLR4 and could therefore act as chaperones for TLR4 or as promoters of LPS internalization.[8][111][112]
Antagonists
editAs of 2020, there were no specific TLR4 antagonists approved as drugs.[113]
- Amitriptyline[114]
- Cyclobenzaprine[114]
- Eritoran[115]
- Ketotifen[114]
- Imipramine[114]
- Mianserin[114]
- Ibudilast[116]
- Pinocembrin[117]
- Resatorvid[118]
- M62812
- Naloxone[119]
- (+)-Naloxone ("unnatural" isomer, lacks opioid receptor affinity so selective for TLR4 inhibition)[105]
- Naltrexone[119]
- (+)-Naltrexone[119]
- LPS-RS[119]
- Propentofylline[citation needed]
- Pentoxifylline[120] (and downregulate TLR4 expression[121])
- Tapentadol (mixed agonist/antagonist)
- TLR4-IN-C34[122]
- Palmitoylethanolamide[123]
References
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000136869 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000039005 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c Vaure C, Liu Y (2014). "A comparative review of toll-like receptor 4 expression and functionality in different animal species". Frontiers in Immunology. 5: 316. doi:10.3389/fimmu.2014.00316. PMC 4090903. PMID 25071777.
- ^ Mahnke K, Becher E, Ricciardi-Castagnoli P, Luger TA, Schwarz T, Grabbe S (1997). "CD14 is Expressed by Subsets of Murine Dendritic Cells and Upregulated by Lipopolysaccharide". In Ricciardi-Castagnoli P (ed.). Dendritic Cells in Fundamental and Clinical Immunology. Advances in Experimental Medicine and Biology. Vol. 417. Boston, MA: Springer US. pp. 145–159. doi:10.1007/978-1-4757-9966-8_25. ISBN 978-1-4757-9968-2. PMID 9286353.
- ^ Sabroe I, Jones EC, Usher LR, Whyte MK, Dower SK (May 2002). "Toll-like receptor (TLR)2 and TLR4 in human peripheral blood granulocytes: a critical role for monocytes in leukocyte lipopolysaccharide responses". Journal of Immunology. 168 (9): 4701–4710. doi:10.4049/jimmunol.168.9.4701. PMID 11971020.
- ^ a b c Yang H, Wang H, Ju Z, Ragab AA, Lundbäck P, Long W, et al. (January 2015). "MD-2 is required for disulfide HMGB1-dependent TLR4 signaling". The Journal of Experimental Medicine. 212 (1): 5–14. doi:10.1084/jem.20141318. PMC 4291531. PMID 25559892.
- ^ a b Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, et al. (November 2005). "Regulation of lung injury and repair by Toll-like receptors and hyaluronan". Nature Medicine. 11 (11): 1173–1179. doi:10.1038/nm1315. PMID 16244651. S2CID 11765495.
- ^ a b Fang H, Ang B, Xu X, Huang X, Wu Y, Sun Y, et al. (March 2014). "TLR4 is essential for dendritic cell activation and anti-tumor T-cell response enhancement by DAMPs released from chemically stressed cancer cells". Cellular & Molecular Immunology. 11 (2): 150–159. doi:10.1038/cmi.2013.59. PMC 4003380. PMID 24362470.
- ^ a b c Hernandez C, Huebener P, Schwabe RF (November 2016). "Damage-associated molecular patterns in cancer: a double-edged sword". Oncogene. 35 (46): 5931–5941. doi:10.1038/onc.2016.104. PMC 5119456. PMID 27086930.
- ^ a b c d e Jang GY, Lee JW, Kim YS, Lee SE, Han HD, Hong KJ, et al. (December 2020). "Interactions between tumor-derived proteins and Toll-like receptors". Experimental & Molecular Medicine. 52 (12): 1926–1935. doi:10.1038/s12276-020-00540-4. PMC 8080774. PMID 33299138.
- ^ a b c d Molteni M, Gemma S, Rossetti C (2016). "The Role of Toll-Like Receptor 4 in Infectious and Noninfectious Inflammation". Mediators of Inflammation. 2016: 6978936. doi:10.1155/2016/6978936. PMC 4887650. PMID 27293318.
- ^ a b Roh JS, Sohn DH (August 2018). "Damage-Associated Molecular Patterns in Inflammatory Diseases". Immune Network. 18 (4): e27. doi:10.4110/in.2018.18.e27. PMC 6117512. PMID 30181915.
- ^ Tsukamoto H, Takeuchi S, Kubota K, Kobayashi Y, Kozakai S, Ukai I, et al. (June 2018). "Lipopolysaccharide (LPS)-binding protein stimulates CD14-dependent Toll-like receptor 4 internalization and LPS-induced TBK1-IKKϵ-IRF3 axis activation". The Journal of Biological Chemistry. 293 (26): 10186–10201. doi:10.1074/jbc.M117.796631. PMC 6028956. PMID 29760187.
- ^ a b Park BS, Song DH, Kim HM, Choi BS, Lee H, Lee JO (April 2009). "The structural basis of lipopolysaccharide recognition by the TLR4-MD-2 complex". Nature. 458 (7242): 1191–1195. Bibcode:2009Natur.458.1191P. doi:10.1038/nature07830. PMID 19252480. S2CID 4396446.
- ^ Park BS, Lee JO (December 2013). "Recognition of lipopolysaccharide pattern by TLR4 complexes". Experimental & Molecular Medicine. 45 (12): e66. doi:10.1038/emm.2013.97. PMC 3880462. PMID 24310172.
- ^ Steimle A, Autenrieth IB, Frick JS (August 2016). "Structure and function: Lipid A modifications in commensals and pathogens". International Journal of Medical Microbiology. 306 (5): 290–301. doi:10.1016/j.ijmm.2016.03.001. PMID 27009633.
- ^ Kelley SL, Lukk T, Nair SK, Tapping RI (February 2013). "The crystal structure of human soluble CD14 reveals a bent solenoid with a hydrophobic amino-terminal pocket". Journal of Immunology. 190 (3): 1304–1311. doi:10.4049/jimmunol.1202446. PMC 3552104. PMID 23264655.
- ^ Muroi M, Tanamoto K (November 2002). "The polysaccharide portion plays an indispensable role in Salmonella lipopolysaccharide-induced activation of NF-kappaB through human toll-like receptor 4". Infection and Immunity. 70 (11): 6043–6047. doi:10.1128/IAI.70.11.6043-6047.2002. PMC 130318. PMID 12379680.
- ^ Cavaillon JM, Fitting C, Caroff M, Haeffner-Cavaillon N (March 1989). "Dissociation of cell-associated interleukin-1 (IL-1) and IL-1 release induced by lipopolysaccharide and lipid A". Infection and Immunity. 57 (3): 791–797. doi:10.1128/iai.57.3.791-797.1989. PMC 313178. PMID 2537258.
- ^ a b c d Shen H, Tesar BM, Walker WE, Goldstein DR (August 2008). "Dual signaling of MyD88 and TRIF is critical for maximal TLR4-induced dendritic cell maturation". Journal of Immunology. 181 (3): 1849–1858. doi:10.4049/jimmunol.181.3.1849. PMC 2507878. PMID 18641322.
- ^ Nakayama M, Niki Y, Kawasaki T, Takeda Y, Ikegami H, Toyama Y, et al. (October 2013). "IL-32-PAR2 axis is an innate immunity sensor providing alternative signaling for LPS-TRIF axis". Scientific Reports. 3 (1): 2960. Bibcode:2013NatSR...3E2960N. doi:10.1038/srep02960. PMC 3797434. PMID 24129891.
- ^ Pridmore AC, Jarvis GA, John CM, Jack DL, Dower SK, Read RC (July 2003). "Activation of toll-like receptor 2 (TLR2) and TLR4/MD2 by Neisseria is independent of capsule and lipooligosaccharide (LOS) sialylation but varies widely among LOS from different strains". Infection and Immunity. 71 (7): 3901–3908. doi:10.1128/IAI.71.7.3901-3908.2003. PMC 161978. PMID 12819075.
- ^ Stephenson HN, John CM, Naz N, Gundogdu O, Dorrell N, Wren BW, et al. (July 2013). "Campylobacter jejuni lipooligosaccharide sialylation, phosphorylation, and amide/ester linkage modifications fine-tune human Toll-like receptor 4 activation". The Journal of Biological Chemistry. 288 (27): 19661–19672. doi:10.1074/jbc.M113.468298. PMC 3707672. PMID 23629657.
- ^ Alexander-Floyd J, Bass AR, Harberts EM, Grubaugh D, Buxbaum JD, Brodsky IE, et al. (August 2022). Bäumler AJ (ed.). "Lipid A Variants Activate Human TLR4 and the Noncanonical Inflammasome Differently and Require the Core Oligosaccharide for Inflammasome Activation". Infection and Immunity. 90 (8): e0020822. doi:10.1128/iai.00208-22. PMC 9387229. PMID 35862709.
- ^ Bonhomme D, Santecchia I, Vernel-Pauillac F, Caroff M, Germon P, Murray G, et al. (August 2020). "Leptospiral LPS escapes mouse TLR4 internalization and TRIF‑associated antimicrobial responses through O antigen and associated lipoproteins". PLOS Pathogens. 16 (8): e1008639. doi:10.1371/journal.ppat.1008639. PMC 7447051. PMID 32790743.
- ^ a b Pålsson-McDermott EM, O'Neill LA (October 2004). "Signal transduction by the lipopolysaccharide receptor, Toll-like receptor-4". Immunology. 113 (2): 153–162. doi:10.1111/j.1365-2567.2004.01976.x. PMC 1782563. PMID 15379975.
- ^ Lu YC, Yeh WC, Ohashi PS (May 2008). "LPS/TLR4 signal transduction pathway". Cytokine. 42 (2): 145–151. doi:10.1016/j.cyto.2008.01.006. PMID 18304834.
- ^ a b Meissner F, Scheltema RA, Mollenkopf HJ, Mann M (April 2013). "Direct proteomic quantification of the secretome of activated immune cells". Science. 340 (6131): 475–478. Bibcode:2013Sci...340..475M. doi:10.1126/science.1232578. PMID 23620052. S2CID 40513139.
- ^ a b Kawai T, Takeuchi O, Fujita T, Inoue J, Mühlradt PF, Sato S, et al. (November 2001). "Lipopolysaccharide stimulates the MyD88-independent pathway and results in activation of IFN-regulatory factor 3 and the expression of a subset of lipopolysaccharide-inducible genes". Journal of Immunology. 167 (10): 5887–5894. doi:10.4049/jimmunol.167.10.5887. PMID 11698465.
- ^ a b Chanteux H, Guisset AC, Pilette C, Sibille Y (October 2007). "LPS induces IL-10 production by human alveolar macrophages via MAPKinases- and Sp1-dependent mechanisms". Respiratory Research. 8 (1): 71. doi:10.1186/1465-9921-8-71. PMC 2080632. PMID 17916230.
- ^ a b Ciesielska A, Matyjek M, Kwiatkowska K (February 2021). "TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling". Cellular and Molecular Life Sciences. 78 (4): 1233–1261. doi:10.1007/s00018-020-03656-y. PMC 7904555. PMID 33057840.
- ^ O'Neill LA, Golenbock D, Bowie AG (June 2013). "The history of Toll-like receptors - redefining innate immunity". Nature Reviews. Immunology. 13 (6): 453–460. doi:10.1038/nri3446. hdl:2262/72552. PMID 23681101. S2CID 205491986.
- ^ Watanabe S, Kumazawa Y, Inoue J (2013). "Liposomal lipopolysaccharide initiates TRIF-dependent signaling pathway independent of CD14". PLOS ONE. 8 (4): e60078. Bibcode:2013PLoSO...860078W. doi:10.1371/journal.pone.0060078. PMC 3615118. PMID 23565187.
- ^ Lien E, Means TK, Heine H, Yoshimura A, Kusumoto S, Fukase K, et al. (February 2000). "Toll-like receptor 4 imparts ligand-specific recognition of bacterial lipopolysaccharide". The Journal of Clinical Investigation. 105 (4): 497–504. doi:10.1172/JCI8541. PMC 289161. PMID 10683379.
- ^ a b Shetab Boushehri MA, Lamprecht A (November 2018). "TLR4-Based Immunotherapeutics in Cancer: A Review of the Achievements and Shortcomings". Molecular Pharmaceutics. 15 (11): 4777–4800. doi:10.1021/acs.molpharmaceut.8b00691. PMID 30226786. S2CID 52297047.
- ^ Kaisho T, Takeuchi O, Kawai T, Hoshino K, Akira S (May 2001). "Endotoxin-induced maturation of MyD88-deficient dendritic cells". Journal of Immunology. 166 (9): 5688–5694. doi:10.4049/jimmunol.166.9.5688. PMID 11313410.
- ^ Hoebe K, Janssen EM, Kim SO, Alexopoulou L, Flavell RA, Han J, et al. (December 2003). "Upregulation of costimulatory molecules induced by lipopolysaccharide and double-stranded RNA occurs by Trif-dependent and Trif-independent pathways". Nature Immunology. 4 (12): 1223–1229. doi:10.1038/ni1010. PMID 14625548. S2CID 8505015.
- ^ Shen H, Tesar BM, Walker WE, Goldstein DR (August 2008). "Dual signaling of MyD88 and TRIF is critical for maximal TLR4-induced dendritic cell maturation". Journal of Immunology. 181 (3): 1849–1858. doi:10.4049/jimmunol.181.3.1849. PMC 2507878. PMID 18641322.
- ^ Trombetta ES, Ebersold M, Garrett W, Pypaert M, Mellman I (February 2003). "Activation of lysosomal function during dendritic cell maturation". Science. 299 (5611): 1400–1403. doi:10.1126/science.1080106. PMID 12610307. S2CID 46594244.
- ^ Turley SJ, Inaba K, Garrett WS, Ebersold M, Unternaehrer J, Steinman RM, et al. (April 2000). "Transport of peptide-MHC class II complexes in developing dendritic cells". Science. 288 (5465): 522–527. doi:10.1126/science.288.5465.522. PMID 10775112.
- ^ Kaisho T, Takeuchi O, Kawai T, Hoshino K, Akira S (May 2001). "Endotoxin-induced maturation of MyD88-deficient dendritic cells". Journal of Immunology. 166 (9): 5688–5694. doi:10.4049/jimmunol.166.9.5688. PMID 11313410.
- ^ Hoebe K, Janssen EM, Kim SO, Alexopoulou L, Flavell RA, Han J, et al. (December 2003). "Upregulation of costimulatory molecules induced by lipopolysaccharide and double-stranded RNA occurs by Trif-dependent and Trif-independent pathways". Nature Immunology. 4 (12): 1223–1229. doi:10.1038/ni1010. PMID 14625548. S2CID 8505015.
- ^ Trombetta ES, Ebersold M, Garrett W, Pypaert M, Mellman I (February 2003). "Activation of lysosomal function during dendritic cell maturation". Science. 299 (5611): 1400–1403. doi:10.1126/science.1080106. PMID 12610307. S2CID 46594244.
- ^ Turley SJ, Inaba K, Garrett WS, Ebersold M, Unternaehrer J, Steinman RM, et al. (April 2000). "Transport of peptide-MHC class II complexes in developing dendritic cells". Science. 288 (5465): 522–527. doi:10.1126/science.288.5465.522. PMID 10775112.
- ^ a b Nair-Gupta P, Baccarini A, Tung N, Seyffer F, Florey O, Huang Y, et al. (July 2014). "TLR signals induce phagosomal MHC-I delivery from the endosomal recycling compartment to allow cross-presentation". Cell. 158 (3): 506–521. doi:10.1016/j.cell.2014.04.054. PMC 4212008. PMID 25083866.
- ^ Han JE, Wui SR, Kim KS, Cho YJ, Cho WJ, Lee NG (2014-01-22). Shin EC (ed.). "Characterization of the structure and immunostimulatory activity of a vaccine adjuvant, de-O-acylated lipooligosaccharide". PLOS ONE. 9 (1): e85838. Bibcode:2014PLoSO...985838H. doi:10.1371/journal.pone.0085838. PMC 3899070. PMID 24465739.
- ^ Sharif O, Bolshakov VN, Raines S, Newham P, Perkins ND (January 2007). "Transcriptional profiling of the LPS induced NF-kappaB response in macrophages". BMC Immunology. 8 (1): 1. doi:10.1186/1471-2172-8-1. PMC 1781469. PMID 17222336.
- ^ Paavonen J, Jenkins D, Bosch FX, Naud P, Salmerón J, Wheeler CM, et al. (June 2007). "Efficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trial". Lancet. 369 (9580): 2161–2170. doi:10.1016/S0140-6736(07)60946-5. PMID 17602732. S2CID 26318328.
- ^ Kundi M (April 2007). "New hepatitis B vaccine formulated with an improved adjuvant system". Expert Review of Vaccines. 6 (2): 133–140. doi:10.1586/14760584.6.2.133. PMID 17408363. S2CID 35472093.
- ^ Garçon N, Di Pasquale A (January 2017). "From discovery to licensure, the Adjuvant System story". Human Vaccines & Immunotherapeutics. 13 (1): 19–33. doi:10.1080/21645515.2016.1225635. PMC 5287309. PMID 27636098.
- ^ Beutler B, Rehli M (2002). "Evolution of the TIR, Tolls and TLRS: Functional Inferences from Computational Biology". Toll-Like Receptor Family Members and Their Ligands. Current Topics in Microbiology and Immunology. Vol. 270. pp. 1–21. doi:10.1007/978-3-642-59430-4_1. ISBN 978-3-642-63975-3. PMID 12467241.
- ^ Smirnova I, Poltorak A, Chan EK, McBride C, Beutler B (2000). "Phylogenetic variation and polymorphism at the toll-like receptor 4 locus (TLR4)". Genome Biology. 1 (1): RESEARCH002. doi:10.1186/gb-2000-1-1-research002. PMC 31919. PMID 11104518.
- ^ Quach H, Wilson D, Laval G, Patin E, Manry J, Guibert J, et al. (December 2013). "Different selective pressures shape the evolution of Toll-like receptors in human and African great ape populations". Human Molecular Genetics. 22 (23): 4829–4840. doi:10.1093/hmg/ddt335. PMC 3820138. PMID 23851028.
- ^ a b Barreiro LB, Ben-Ali M, Quach H, Laval G, Patin E, Pickrell JK, et al. (July 2009). "Evolutionary dynamics of human Toll-like receptors and their different contributions to host defense". PLOS Genetics. 5 (7): e1000562. doi:10.1371/journal.pgen.1000562. PMC 2702086. PMID 19609346.
- ^ Plantinga TS, Ioana M, Alonso S, Izagirre N, Hervella M, Joosten LA, et al. (2012). "The evolutionary history of TLR4 polymorphisms in Europe". Journal of Innate Immunity. 4 (2): 168–175. doi:10.1159/000329492. PMC 6741577. PMID 21968286.
- ^ Noreen M, Shah MA, Mall SM, Choudhary S, Hussain T, Ahmed I, et al. (March 2012). "TLR4 polymorphisms and disease susceptibility". Inflammation Research. 61 (3): 177–188. doi:10.1007/s00011-011-0427-1. PMID 22277994. S2CID 9500302.
- ^ Long H, O'Connor BP, Zemans RL, Zhou X, Yang IV, Schwartz DA (2014-04-02). "The Toll-like receptor 4 polymorphism Asp299Gly but not Thr399Ile influences TLR4 signaling and function". PLOS ONE. 9 (4): e93550. Bibcode:2014PLoSO...993550L. doi:10.1371/journal.pone.0093550. PMC 3973565. PMID 24695807.
- ^ Figueroa L, Xiong Y, Song C, Piao W, Vogel SN, Medvedev AE (May 2012). "The Asp299Gly polymorphism alters TLR4 signaling by interfering with recruitment of MyD88 and TRIF". Journal of Immunology. 188 (9): 4506–4515. doi:10.4049/jimmunol.1200202. PMC 3531971. PMID 22474023.
- ^ Ohto U, Yamakawa N, Akashi-Takamura S, Miyake K, Shimizu T (November 2012). "Structural analyses of human Toll-like receptor 4 polymorphisms D299G and T399I". The Journal of Biological Chemistry. 287 (48): 40611–40617. doi:10.1074/jbc.M112.404608. PMC 3504774. PMID 23055527.
- ^ Akira S, Takeda K (July 2004). "Toll-like receptor signalling". Nature Reviews. Immunology. 4 (7): 499–511. doi:10.1038/nri1391. PMID 15229469.
- ^ Netea MG, Wijmenga C, O'Neill LA (May 2012). "Genetic variation in Toll-like receptors and disease susceptibility". Nature Immunology. 13 (6): 535–542. doi:10.1038/ni.2284. PMID 22610250. S2CID 24438756.
- ^ Chettab K, Fitzsimmons C, Novikov A, Denis M, Phelip C, Mathé D, et al. (2023). "A systemically administered detoxified TLR4 agonist displays potent antitumor activity and an acceptable tolerance profile in preclinical models". Frontiers in Immunology. 14: 1066402. doi:10.3389/fimmu.2023.1066402. PMC 10200957. PMID 37223101.
- ^ Richert I, Berchard P, Abbes L, Novikov A, Chettab K, Vandermoeten A, et al. (September 2023). "A TLR4 Agonist Induces Osteosarcoma Regression by Inducing an Antitumor Immune Response and Reprogramming M2 Macrophages to M1 Macrophages". Cancers. 15 (18): 4635. doi:10.3390/cancers15184635. PMC 10526955. PMID 37760603.
- ^ Maruyama K, Selmani Z, Ishii H, Yamaguchi K (March 2011). "Innate immunity and cancer therapy". International Immunopharmacology. 11 (3): 350–357. doi:10.1016/j.intimp.2010.09.012. PMID 20955832.
- ^ Starnes CO (May 1992). "Coley's toxins in perspective". Nature. 357 (6373): 11–12. Bibcode:1992Natur.357...11S. doi:10.1038/357011a0. PMID 1574121. S2CID 4265230.
- ^ Tsuji S, Matsumoto M, Takeuchi O, Akira S, Azuma I, Hayashi A, et al. (December 2000). Kaufmann SH (ed.). "Maturation of human dendritic cells by cell wall skeleton of Mycobacterium bovis bacillus Calmette-Guérin: involvement of toll-like receptors". Infection and Immunity. 68 (12): 6883–6890. doi:10.1128/IAI.68.12.6883-6890.2000. PMC 97794. PMID 11083809.
- ^ Ryoma Y, Moriya Y, Okamoto M, Kanaya I, Saito M, Sato M (2004-09-01). "Biological effect of OK-432 (picibanil) and possible application to dendritic cell therapy". Anticancer Research. 24 (5C): 3295–3301. PMID 15515424.
- ^ Okamoto M, Oshikawa T, Tano T, Ohe G, Furuichi S, Nishikawa H, et al. (February 2003). "Involvement of Toll-like receptor 4 signaling in interferon-gamma production and antitumor effect by streptococcal agent OK-432". Journal of the National Cancer Institute. 95 (4): 316–326. doi:10.1093/jnci/95.4.316. PMID 12591988.
- ^ Shear MB, Perrault M (April 1944). "Chemical Treatment of Tumors. IX. Reactions of Mice with Primary Subcutaneous Tumors to Injection of a Hemorrhage-Producing Bacterial Polysaccharide1". JNCI: Journal of the National Cancer Institute. 4 (5): 461–476. doi:10.1093/jnci/4.5.461.
- ^ Berendt MJ, North RJ, Kirstein DP (December 1978). "The immunological basis of endotoxin-induced tumor regression. Requirement for a pre-existing state of concomitant anti-tumor immunity". The Journal of Experimental Medicine. 148 (6): 1560–1569. doi:10.1084/jem.148.6.1560. PMC 2185097. PMID 309922.
- ^ Engelhardt R, Mackensen A, Galanos C (May 1991). "Phase I trial of intravenously administered endotoxin (Salmonella abortus equi) in cancer patients". Cancer Research. 51 (10): 2524–2530. PMID 2021932.
- ^ "Melacine - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2024-02-20.
- ^ Bhatia S, Miller NJ, Lu H, Longino NV, Ibrani D, Shinohara MM, et al. (February 2019). "Intratumoral G100, a TLR4 Agonist, Induces Antitumor Immune Responses and Tumor Regression in Patients with Merkel Cell Carcinoma". Clinical Cancer Research. 25 (4): 1185–1195. doi:10.1158/1078-0432.CCR-18-0469. PMC 6368904. PMID 30093453.
- ^ Halwani AS, Panizo C, Isufi I, Herrera AF, Okada CY, Cull EH, et al. (April 2022). "Phase 1/2 study of intratumoral G100 (TLR4 agonist) with or without pembrolizumab in follicular lymphoma". Leukemia & Lymphoma. 63 (4): 821–833. doi:10.1080/10428194.2021.2010057. PMID 34865586. S2CID 244943266.
- ^ a b Flowers C, Panizo C, Isufi I, Herrera AF, Okada C, Cull EH, et al. (2017-12-08). "Intratumoral G100 Induces Systemic Immunity and Abscopal Tumor Regression in Patients with Follicular Lymphoma: Results of a Phase 1/ 2 Study Examining G100 Alone and in Combination with Pembrolizumab". Blood. 130: 2771. doi:10.1182/blood.V130.Suppl_1.2771.2771 (inactive 1 November 2024). ISSN 0006-4971.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Rajput S, Volk-Draper LD, Ran S (August 2013). "TLR4 is a novel determinant of the response to paclitaxel in breast cancer". Molecular Cancer Therapeutics. 12 (8): 1676–1687. doi:10.1158/1535-7163.MCT-12-1019. PMC 3742631. PMID 23720768.
- ^ Zhang R, Zhao J, Xu J, Jiao DX, Wang J, Gong ZQ, et al. (October 2017). "Andrographolide suppresses proliferation of human colon cancer SW620 cells through the TLR4/NF-κB/MMP-9 signaling pathway". Oncology Letters. 14 (4): 4305–4310. doi:10.3892/ol.2017.6669. PMC 5604146. PMID 28943944.
- ^ Wang CH, Wang PJ, Hsieh YC, Lo S, Lee YC, Chen YC, et al. (February 2018). "Resistin facilitates breast cancer progression via TLR4-mediated induction of mesenchymal phenotypes and stemness properties". Oncogene. 37 (5): 589–600. doi:10.1038/onc.2017.357. PMID 28991224. S2CID 24926622.
- ^ Kelly MG, Alvero AB, Chen R, Silasi DA, Abrahams VM, Chan S, et al. (April 2006). "TLR-4 signaling promotes tumor growth and paclitaxel chemoresistance in ovarian cancer". Cancer Research. 66 (7): 3859–3868. doi:10.1158/0008-5472.CAN-05-3948. PMID 16585214.
- ^ Khademalhosseini M, Arababadi MK (May 2019). "Toll-like receptor 4 and breast cancer: an updated systematic review". Breast Cancer. 26 (3): 265–271. doi:10.1007/s12282-018-00935-2. PMID 30543015. S2CID 56143069.
- ^ Zhu L, Yuan H, Jiang T, Wang R, Ma H, Zhang S (2013-12-20). "Association of TLR2 and TLR4 polymorphisms with risk of cancer: a meta-analysis". PLOS ONE. 8 (12): e82858. Bibcode:2013PLoSO...882858Z. doi:10.1371/journal.pone.0082858. PMC 3869723. PMID 24376595.
- ^ Wardill HR, Van Sebille YZ, Mander KA, Gibson RJ, Logan RM, Bowen JM, et al. (February 2015). "Toll-like receptor 4 signaling: a common biological mechanism of regimen-related toxicities: an emerging hypothesis for neuropathy and gastrointestinal toxicity". Cancer Treatment Reviews. 41 (2): 122–128. doi:10.1016/j.ctrv.2014.11.005. PMID 25512119.
- ^ Tahara K, Kim HD, Jin JJ, Maxwell JA, Li L, Fukuchi K (November 2006). "Role of toll-like receptor signalling in Abeta uptake and clearance". Brain. 129 (Pt 11): 3006–3019. doi:10.1093/brain/awl249. PMC 2445613. PMID 16984903.
- ^ a b Buchanan MM, Hutchinson M, Watkins LR, Yin H (July 2010). "Toll-like receptor 4 in CNS pathologies". Journal of Neurochemistry. 114 (1): 13–27. doi:10.1111/j.1471-4159.2010.06736.x. PMC 2909662. PMID 20402965.
- ^ Qin Y, Liu Y, Hao W, Decker Y, Tomic I, Menger MD, et al. (October 2016). "Stimulation of TLR4 Attenuates Alzheimer's Disease-Related Symptoms and Pathology in Tau-Transgenic Mice". Journal of Immunology. 197 (8): 3281–3292. doi:10.4049/jimmunol.1600873. PMID 27605009.
- ^ Gambuzza M, Licata N, Palella E, Celi D, Foti Cuzzola V, Italiano D, et al. (October 2011). "Targeting Toll-like receptors: emerging therapeutics for multiple sclerosis management". Journal of Neuroimmunology. 239 (1–2): 1–12. doi:10.1016/j.jneuroim.2011.08.010. PMID 21889214. S2CID 3277551.
- ^ Rannikko EH, Weber SS, Kahle PJ (September 2015). "Exogenous α-synuclein induces toll-like receptor 4 dependent inflammatory responses in astrocytes". BMC Neuroscience. 16: 57. doi:10.1186/s12868-015-0192-0. PMC 4562100. PMID 26346361.
- ^ Walter S, Letiembre M, Liu Y, Heine H, Penke B, Hao W, et al. (2007). "Role of the toll-like receptor 4 in neuroinflammation in Alzheimer's disease". Cellular Physiology and Biochemistry. 20 (6): 947–956. doi:10.1159/000110455. PMID 17982277. S2CID 6752610.
- ^ Land WG (February 2015). "The Role of Damage-Associated Molecular Patterns in Human Diseases: Part I - Promoting inflammation and immunity". Sultan Qaboos University Medical Journal. 15 (1): e9 – e21. PMC 4318613. PMID 25685392.
- ^ Festoff BW, Sajja RK, van Dreden P, Cucullo L (August 2016). "HMGB1 and thrombin mediate the blood-brain barrier dysfunction acting as biomarkers of neuroinflammation and progression to neurodegeneration in Alzheimer's disease". Journal of Neuroinflammation. 13 (1): 194. doi:10.1186/s12974-016-0670-z. PMC 4995775. PMID 27553758.
- ^ Chaves ML, Camozzato AL, Ferreira ED, Piazenski I, Kochhann R, Dall'Igna O, et al. (January 2010). "Serum levels of S100B and NSE proteins in Alzheimer's disease patients". Journal of Neuroinflammation. 7: 6. doi:10.1186/1742-2094-7-6. PMC 2832635. PMID 20105309.
- ^ Yang Y, Han C, Guo L, Guan Q (April 2018). "High expression of the HMGB1-TLR4 axis and its downstream signaling factors in patients with Parkinson's disease and the relationship of pathological staging". Brain and Behavior. 8 (4): e00948. doi:10.1002/brb3.948. PMC 5893335. PMID 29670828.
- ^ Wu L, Xian X, Xu G, Tan Z, Dong F, Zhang M, et al. (2022-08-21). "Toll-Like Receptor 4: A Promising Therapeutic Target for Alzheimer's Disease". Mediators of Inflammation. 2022: 7924199. doi:10.1155/2022/7924199. PMC 9420645. PMID 36046763.
- ^ a b Leitner GR, Wenzel TJ, Marshall N, Gates EJ, Klegeris A (October 2019). "Targeting toll-like receptor 4 to modulate neuroinflammation in central nervous system disorders". Expert Opinion on Therapeutic Targets. 23 (10): 865–882. doi:10.1080/14728222.2019.1676416. PMID 31580163. S2CID 203652175.
- ^ Michaud JP, Hallé M, Lampron A, Thériault P, Préfontaine P, Filali M, et al. (January 2013). "Toll-like receptor 4 stimulation with the detoxified ligand monophosphoryl lipid A improves Alzheimer's disease-related pathology". Proceedings of the National Academy of Sciences of the United States of America. 110 (5): 1941–1946. Bibcode:2013PNAS..110.1941M. doi:10.1073/pnas.1215165110. PMC 3562771. PMID 23322736.
- ^ Shavit Y, Wolf G, Goshen I, Livshits D, Yirmiya R (May 2005). "Interleukin-1 antagonizes morphine analgesia and underlies morphine tolerance". Pain. 115 (1–2): 50–59. doi:10.1016/j.pain.2005.02.003. PMID 15836969. S2CID 7286123.
- ^ Mohan S, Davis RL, DeSilva U, Stevens CW (October 2010). "Dual regulation of mu opioid receptors in SK-N-SH neuroblastoma cells by morphine and interleukin-1β: evidence for opioid-immune crosstalk". Journal of Neuroimmunology. 227 (1–2): 26–34. doi:10.1016/j.jneuroim.2010.06.007. PMC 2942958. PMID 20615556.
- ^ Komatsu T, Sakurada S, Katsuyama S, Sanai K, Sakurada T (2009). Mechanism of allodynia evoked by intrathecal morphine-3-glucuronide in mice. International Review of Neurobiology. Vol. 85. pp. 207–19. doi:10.1016/S0074-7742(09)85016-2. ISBN 978-0-12-374893-5. PMID 19607972.
- ^ Lewis SS, Hutchinson MR, Rezvani N, Loram LC, Zhang Y, Maier SF, et al. (January 2010). "Evidence that intrathecal morphine-3-glucuronide may cause pain enhancement via toll-like receptor 4/MD-2 and interleukin-1beta". Neuroscience. 165 (2): 569–583. doi:10.1016/j.neuroscience.2009.10.011. PMC 2795035. PMID 19833175.
- ^ Shen CH, Tsai RY, Shih MS, Lin SL, Tai YH, Chien CC, et al. (February 2011). "Etanercept restores the antinociceptive effect of morphine and suppresses spinal neuroinflammation in morphine-tolerant rats". Anesthesia and Analgesia. 112 (2): 454–459. doi:10.1213/ANE.0b013e3182025b15. PMID 21081778. S2CID 12295407.
- ^ Hook MA, Washburn SN, Moreno G, Woller SA, Puga D, Lee KH, et al. (February 2011). "An IL-1 receptor antagonist blocks a morphine-induced attenuation of locomotor recovery after spinal cord injury". Brain, Behavior, and Immunity. 25 (2): 349–359. doi:10.1016/j.bbi.2010.10.018. PMC 3025088. PMID 20974246.
- ^ Watkins LR, Hutchinson MR, Rice KC, Maier SF (November 2009). "The "toll" of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia". Trends in Pharmacological Sciences. 30 (11): 581–591. doi:10.1016/j.tips.2009.08.002. PMC 2783351. PMID 19762094.
- ^ a b c Hutchinson MR, Zhang Y, Brown K, Coats BD, Shridhar M, Sholar PW, et al. (July 2008). "Non-stereoselective reversal of neuropathic pain by naloxone and naltrexone: involvement of toll-like receptor 4 (TLR4)". The European Journal of Neuroscience. 28 (1): 20–29. doi:10.1111/j.1460-9568.2008.06321.x. PMC 2588470. PMID 18662331.
- ^ Hutchinson MR, Coats BD, Lewis SS, Zhang Y, Sprunger DB, Rezvani N, et al. (November 2008). "Proinflammatory cytokines oppose opioid-induced acute and chronic analgesia". Brain, Behavior, and Immunity. 22 (8): 1178–1189. doi:10.1016/j.bbi.2008.05.004. PMC 2783238. PMID 18599265.
- ^ Hutchinson MR, Lewis SS, Coats BD, Rezvani N, Zhang Y, Wieseler JL, et al. (May 2010). "Possible involvement of toll-like receptor 4/myeloid differentiation factor-2 activity of opioid inactive isomers causes spinal proinflammation and related behavioral consequences". Neuroscience. 167 (3): 880–893. doi:10.1016/j.neuroscience.2010.02.011. PMC 2854318. PMID 20178837.
- ^ Lin SL, Tsai RY, Tai YH, Cherng CH, Wu CT, Yeh CC, et al. (February 2010). "Ultra-low dose naloxone upregulates interleukin-10 expression and suppresses neuroinflammation in morphine-tolerant rat spinal cords". Behavioural Brain Research. 207 (1): 30–36. doi:10.1016/j.bbr.2009.09.034. PMID 19799935. S2CID 5128970.
- ^ "Neuroscience: Making morphine work better". Nature. 484 (7395): 419. 26 April 2012. Bibcode:2012Natur.484Q.419.. doi:10.1038/484419a. S2CID 52805136.
- ^ Drahl C (22 August 2012). "Small Molecules Target Toll-Like Receptors". Chemical & Engineering News.
- ^ Manček-Keber M, Jerala R (February 2015). "Postulates for validating TLR4 agonists". European Journal of Immunology. 45 (2): 356–370. doi:10.1002/eji.201444462. PMID 25476977. S2CID 32029412.
- ^ Kim HM, Kim YM (October 2018). "HMGB1: LPS Delivery Vehicle for Caspase-11-Mediated Pyroptosis". Immunity. 49 (4): 582–584. doi:10.1016/j.immuni.2018.09.021. PMID 30332623.
- ^ Romerio A, Peri F (2020). "Increasing the Chemical Variety of Small-Molecule-Based TLR4 Modulators: An Overview". Frontiers in Immunology. 11: 1210. doi:10.3389/fimmu.2020.01210. PMC 7381287. PMID 32765484.
- ^ a b c d e Hutchinson MR, Loram LC, Zhang Y, Shridhar M, Rezvani N, Berkelhammer D, et al. (June 2010). "Evidence that tricyclic small molecules may possess toll-like receptor and myeloid differentiation protein 2 activity". Neuroscience. 168 (2): 551–563. doi:10.1016/j.neuroscience.2010.03.067. PMC 2872682. PMID 20381591.
- ^ Chen F, Zou L, Williams B, Chao W (November 2021). "Targeting Toll-Like Receptors in Sepsis: From Bench to Clinical Trials". Antioxidants & Redox Signaling. 35 (15): 1324–1339. doi:10.1089/ars.2021.0005. PMC 8817700. PMID 33588628.
- ^ Jia ZJ, Wu FX, Huang QH, Liu JM (April 2012). "[Toll-like receptor 4: the potential therapeutic target for neuropathic pain]". Zhongguo Yi Xue Ke Xue Yuan Xue Bao. Acta Academiae Medicinae Sinicae. 34 (2): 168–173. doi:10.3881/j.issn.1000-503X.2012.02.013. PMID 22776604.
- ^ Lan X, Han X, Li Q, Li Q, Gao Y, Cheng T, et al. (March 2017). "Pinocembrin protects hemorrhagic brain primarily by inhibiting toll-like receptor 4 and reducing M1 phenotype microglia". Brain, Behavior, and Immunity. 61: 326–339. doi:10.1016/j.bbi.2016.12.012. PMC 5453178. PMID 28007523.
- ^ Kaieda A, Takahashi M, Fukuda H, Okamoto R, Morimoto S, Gotoh M, et al. (December 2019). "Structure-Based Design, Synthesis, and Biological Evaluation of Imidazo[4,5-b]Pyridin-2-one-Based p38 MAP Kinase Inhibitors: Part 2". ChemMedChem. 14 (24): 2093–2101. doi:10.1002/cmdc.201900373. PMID 31697454. S2CID 207951964.
- ^ a b c d Hutchinson MR, Zhang Y, Shridhar M, Evans JH, Buchanan MM, Zhao TX, et al. (January 2010). "Evidence that opioids may have toll-like receptor 4 and MD-2 effects". Brain, Behavior, and Immunity. 24 (1): 83–95. doi:10.1016/j.bbi.2009.08.004. PMC 2788078. PMID 19679181.
- ^ Speer EM, Dowling DJ, Ozog LS, Xu J, Yang J, Kennady G, et al. (May 2017). "Pentoxifylline inhibits TLR- and inflammasome-mediated in vitro inflammatory cytokine production in human blood with greater efficacy and potency in newborns". Pediatric Research. 81 (5): 806–816. doi:10.1038/pr.2017.6. PMID 28072760. S2CID 47210724.
- ^ Schüller SS, Wisgrill L, Herndl E, Spittler A, Förster-Waldl E, Sadeghi K, et al. (August 2017). "Pentoxifylline modulates LPS-induced hyperinflammation in monocytes of preterm infants in vitro". Pediatric Research. 82 (2): 215–225. doi:10.1038/pr.2017.41. PMID 28288151. S2CID 24897100.
- ^ Neal MD, Jia H, Eyer B, Good M, Guerriero CJ, Sodhi CP, et al. (2013). "Discovery and validation of a new class of small molecule Toll-like receptor 4 (TLR4) inhibitors". PLOS ONE. 8 (6): e65779. Bibcode:2013PLoSO...865779N. doi:10.1371/journal.pone.0065779. PMC 3680486. PMID 23776545.
- ^ Impellizzeri D, Campolo M, Di Paola R, Bruschetta G, de Stefano D, Esposito E, et al. (2015). "Ultramicronized palmitoylethanolamide reduces inflammation an a Th1-mediated model of colitis". European Journal of Inflammation. 13: 14–31. doi:10.1177/1721727X15575869. S2CID 79398556.
External links
edit- Toll-Like+Receptor+4 at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: O00206 (Toll-like receptor 4) at the PDBe-KB.