Toxic vacuolation, also known as toxic vacuolization,[1] is the formation of vacuoles in the cytoplasm of neutrophils in response to severe infections or inflammatory conditions.[2][3]
| Toxic vacuolation | |
|---|---|
| Other names | Toxic vacuolization |
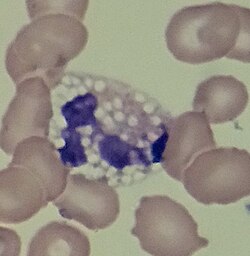 | |
| A vacuolated neutrophil | |
| Specialty | Hematology |
| Causes | Sepsis, bacterial infection, alcohol toxicity, liver failure, G-CSF treatment |
Clinical significance
editToxic vacuolation is associated with sepsis, particularly when accompanied by toxic granulation.[4] The finding is also associated with bacterial infection,[3] alcohol toxicity, liver failure,[4] and treatment with granulocyte colony-stimulating factor, a cytokine drug used to increase the absolute neutrophil count in patients with neutropenia.[5][6]
The formation of toxic vacuoles represents increased phagocytic activity, which is stimulated by the release of cytokines in response to inflammation or tissue injury. Toxic vacuolation frequently occurs in conjunction with toxic granulation and Döhle bodies in inflammatory states, and these findings are collectively referred to as toxic changes.[5] Neutrophilia and left shift (the presence of immature neutrophil precursors such as band neutrophils and metamyelocytes in the peripheral blood) often accompany toxic changes, as these phenomena also occur in response to inflammation.[1][5]
It has been suggested that neutrophil vacuoles not be labelled "toxic vacuoles" unless they are accompanied by other toxic changes, as vacuolation can occur in other conditions.[7]
Similar conditions
editVacuoles may form in neutrophils if a blood sample is left standing for several hours prior to blood smear preparation, but this is an artifactual change with no clinical significance.[4] Artifactual vacuoles are small and of uniform size and distribution, in contrast to toxic vacuoles whose size and placement are variable.[1] Individuals with neutral lipid storage disease may exhibit persistent lipid-filled vacuoles in neutrophils and other granulocytes, which is a distinct phenomenon termed Jordans' anomaly.[8]
See also
editReferences
edit- ^ a b c Betty Ciesla (27 November 2018). "Chapter 10: Abnormalities of white blood cells: quantitative, qualitative and the lipid storage diseases". Hematology in Practice. F.A. Davis. p. 153. ISBN 978-0-8036-6825-6.
- ^ Mary Louise Turgeon (14 April 2014). "Leukocytes and platelets". Linne & Ringsrud's Clinical Laboratory Science - E-Book: The Basics and Routine Techniques (6th ed.). Elsevier Health Sciences. p. 318. ISBN 978-0-323-29280-1.
- ^ a b Barbara J. Bain (11 November 2014). "Chapter 3: Morphology of blood cells". Blood Cells: A Practical Guide (5 ed.). Wiley. pp. 112–113. ISBN 978-1-118-81729-2.
- ^ a b c Barbara J. Bain; Imelda Bates; Mike A Laffan (11 August 2016). "Chapter 5: Blood cell morphology in health and disease". Dacie and Lewis Practical Haematology. Elsevier Health Sciences. p. 93. ISBN 978-0-7020-6925-3.
- ^ a b c "Toxic change". eClinPath. Cornell University College of Veterinary Medicine. 2013. Retrieved 2019-06-28.
- ^ Medscape (23 April 2019). "Neupogen, Granix, Zarxio, Nivestym (filgrastim, tbo-filgrastim, filgrastim-sndz, filgrastim-aafi, G-CSF) dosing, indications, interactions, adverse effects, and more". Medscape Reference. Archived from the original on 13 May 2019. Retrieved 13 July 2019.
- ^ Hematology and Clinical Microscopy Committee (2019). "Blood cell identification: Granulocytes and Monocytes: Neutrophil, toxic" (PDF). Hematology and Clinical Microscopy Glossary. College of American Pathologists. Archived (PDF) from the original on 2019-06-28. Retrieved 2019-06-28.
- ^ John P. Greer; Sherrie L. Perkins (December 2008). "Chapter 62: Qualitative disorders of leukocytes". Wintrobe's Clinical Hematology. Vol. 1 (12th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. p. 1552. ISBN 978-0-7817-6507-7.