This article may require cleanup to meet Wikipedia's quality standards. The specific problem is: Wikipedia is not a "how to" guide. (October 2020) |
Suction Assisted Laryngoscopy Airway Decontamination (SALAD) is incremental step-wise approach to the management of a massively contaminated airway.[1]
Emergency airway management is often complicated by the presence of blood, emesis or other contaminants in the airway. For example, in out-of-hospital cardiac arrest (OHCA), vomiting and regurgitation have a reported incidence of 20–30%.[2][3] The traditional approach to the contaminated airway involves suctioning the airway and repositioning the patient, which can effectively manage airway soiling in many, but not all, cases.[4][5] However, traditional airway management education has not included the integration of a simultaneous suctioning and airway decontamination skill set as a technique that can be deployed in the setting of large volume contamination and clinicians frequently underestimate the importance of suction as part of airway management.[1][6][7]
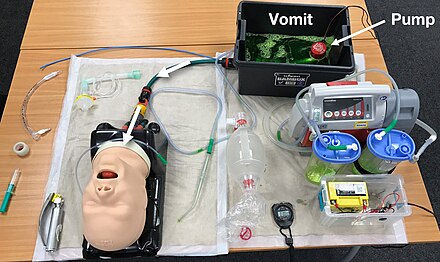
This has led to the development of the SALAD technique, and the creation of modified airway manikins to allow for practice in these techniques.[8]
History
editSALAD was developed as a simulation exercise in 2014, by a US anaesthetist Dr. Jim DuCanto. It was subsequently introduced into several US academic emergency medicine departments, culminating in its presentation at the 2015 Social Media and Critical Care Conference (SMACC). This raised the profile of the technique internationally. Following its introduction to the international community at SMACC, multiple medical educators introduced the technique in their own institutions and services across Australasia, Europe and Asia.
Technique
editThe following description of the SALAD Technique is intended to provide a template for medical educators to practice this technique in a medical simulation setting, and does not constitute medical advice. Wikipedia does not generally approve of articles that serve as guides to perform procedures, however, many medical educators who wish to disseminate information regarding new and effective techniques to manage contaminated airways have sought a template upon which to build their simulation instructions, and this guide to the technique simply serves to provide that template.
The SALAD technique consists of the following steps:[1][8]
| Step | Description | |
|---|---|---|
| 1. | Optimally position the patient to maximise the probability of intubation success (e.g. external auditory meatus level with sternal notch). | |
| 2. | Hold the suction catheter (wide-bore, rigid) in a clenched-fisted right hand, with the distal end of the catheter pointing caudad and posterior, to enable manipulation of the tongue and mandible as required. The curve of the rigid suction catheter should mirror the curve of the structures of the upper airway | |
| 3. | Lead with suction to enable identification of relevant anatomical structure (posterior portion of tongue, epiglottis, vallecular and laryngeal outlet) and follow with the laryngoscope (particularly important with video laryngoscopes to avoid contaminating the optics). | |
| 4. | In order to facilitate placement of the tracheal tube, the suction catheter is moved across to the left side of the mouth and the suction catheter 'parked' in the top of the oesophagus to provide continuous suction during the remainder of the intubation attempt. This can be achieved either by sliding the catheter under the laryngoscope blade, or by briefly removing the catheter and inserting it to the left of the laryngoscope blade. | |
| 5. | Insert the index finger of the right hand into the right-hand side of the oropharynx to create a 'channel' for tracheal tube delivery (known as the SALAD poke). | |
| 6. | Intubate as normal, with or without a bougie. | |
| 7. | Inflate the cuff on the tracheal tube to prevent further contamination of the lower airway. | |
| 8. | suction down the tracheal tube with a flexible suction catheter prior to ventilation to remove any residual contaminant prior to ventilation. |
Note that these images are using a hand-operated suction device, but the principle for motorised suction is the same.
SALAD research
editTo date, there have been no large, randomised controlled trials (RCTs) of SALAD versus conventional emergency airway management strategies in real patients. The sporadic incidence of massive airway contamination during intubation attempts mean that an RCT of SALAD versus usual care is likely to be unfeasible to conduct. However, there is a growing body of lower quality evidence (simulation studies, and studies utilising observational data from patients) that are encouraging in terms of increasing clinician's confidence in managing severely contaminated airways [8][9] and improving intubation success rates as well as time to successful intubation [10][11][12][13] in cases of significant airway soiling. Two case reports in the peer-reviewed literature to date (Summer 2021) have described the SALAD technique as instrumental for emergency airway management in critically ill patients.[14][15]
References
edit- ^ a b c Root, Christopher W.; Mitchell, Oscar J. L.; Brown, Russ; Evers, Christopher B.; Boyle, Jess; Griffin, Cynthia; West, Frances Mae; Gomm, Edward; Miles, Edward; McGuire, Barry; Swaminathan, Anand; St George, Jonathan; Horowitz, James M.; DuCanto, James (2020-03-01). "Suction Assisted Laryngoscopy and Airway Decontamination (SALAD): A technique for improved emergency airway management". Resuscitation Plus. 1–2: 100005. doi:10.1016/j.resplu.2020.100005. ISSN 2666-5204. PMC 8244406. PMID 34223292.
- ^ (Simons, Reed W.; Rea, Thomas D.; Becker, Linda J.; Eisenberg, Mickey S. (2007-09-01). "The incidence and significance of emesis associated with out-of-hospital cardiac arrest". Resuscitation. 74 (3): 427–431. doi:10.1016/j.resuscitation.2007.01.038. ISSN 0300-9572. PMID 17433526.
- ^ Voss, Sarah; Rhys, Megan; Coates, David; Greenwood, Rosemary; Nolan, Jerry P.; Thomas, Matthew; Benger, Jonathan (2014-12-01). "How do paramedics manage the airway during out of hospital cardiac arrest?". Resuscitation. 85 (12): 1662–1666. doi:10.1016/j.resuscitation.2014.09.008. ISSN 0300-9572. PMC 4265730. PMID 25260723. Retrieved 2019-03-04.
- ^ Robinson, Michael; Davidson, Andrew (2014-08-01). "Aspiration under anaesthesia: risk assessment and decision-making". Continuing Education in Anaesthesia, Critical Care & Pain. 14 (4): 171–175. doi:10.1093/bjaceaccp/mkt053. ISSN 1743-1816. Retrieved 2020-10-25.
- ^ Kluger, M. T.; Visvanathan, T.; Myburgh, J. A.; Westhorpe, R. N. (2005-06-01). "Crisis management during anaesthesia: regurgitation, vomiting, and aspiration". BMJ Quality & Safety. 14 (3): –4–e4. doi:10.1136/qshc.2002.004259. ISSN 2044-5415. PMC 1744032. PMID 15933301.
- ^ Prekker, Matthew E.; Kwok, Heemun; Shin, Jenny; Carlbom, David; Grabinsky, Andreas; Rea, Thomas D. (2014-06-01). "The Process of Prehospital Airway Management: Challenges and Solutions During Paramedic Endotracheal Intubation". Critical Care Medicine. 42 (6): 1372–1378. doi:10.1097/CCM.0000000000000213. ISSN 0090-3493. PMC 4902016. PMID 24589641.
- ^ Kozak, Richard J.; Ginther, Bret E.; Bean, Walter S. (1997-01-01). "Difficulties with portable suction equipment used for prehospital advanced airway procedures". Prehospital Emergency Care. 1 (2): 91–95. doi:10.1080/10903129708958795. ISSN 1090-3127. PMID 9709345. Retrieved 2020-10-25.
- ^ a b c DuCanto, James; Serrano, Karen; Thompson, Ryan (2017-01-19). "Novel Airway Training Tool that Simulates Vomiting: Suction-Assisted Laryngoscopy Assisted Decontamination (SALAD) System". Western Journal of Emergency Medicine. 18 (1): 117–120. doi:10.5811/westjem.2016.9.30891. ISSN 1936-9018. PMC 5226742. PMID 28116021. S2CID 24288617.
- ^ Della Vella, Carmine; Thompson, Ryan J.; Serrano, Karen; Riess, Matthias L.; Ducanto, James (2018-12-01). "Suction-Assisted Laryngoscopy-Assisted Decontamination (SALAD) simulator for difficult airway management". Trends in Anaesthesia and Critical Care. 23: 32. doi:10.1016/j.tacc.2018.09.060. ISSN 2210-8440. S2CID 81284308. Retrieved 2020-10-25.
- ^ Pilbery, Richard; Teare, M. Dawn (2019-06-01). "Soiled airway tracheal intubation and the effectiveness of decontamination by paramedics (SATIATED): a randomised controlled manikin study". British Paramedic Journal. 4 (1): 14–21. doi:10.29045/14784726.2019.06.4.1.14. ISSN 1478-4726. PMC 7706770. PMID 33328824.
- ^ Lin, Li-Wei; Huang, Chi-Chieh; Ong, Jiann Ruey; Chong, Chee-Fah; Wu, Nai-Yuan; Hung, Shih-Wen (2019-11-15). "The suction-assisted laryngoscopy assisted decontamination technique toward successful intubation during massive vomiting simulation". Medicine. 98 (46): e17898. doi:10.1097/MD.0000000000017898. ISSN 0025-7974. PMC 6867733. PMID 31725637.
- ^ Ko, Shing; Wong, Oi Fung; Wong, Ching Hin Kevin; Ma, Hing Man; Lit, Chau Hung Albert (2019-11-04). "A pilot study on using Suction-Assisted Laryngoscopy Airway Decontamination techniques to assist endotracheal intubation by GlideScope® in a manikin simulating massive hematemesis". Hong Kong Journal of Emergency Medicine. 28 (5): 305–313. doi:10.1177/1024907919884206. ISSN 1024-9079.
- ^ Jensen, Matthew; Barmaan, Benjamin; Orndahl, Christine M.; Louka, Amir (2020-03-01). "Impact of Suction-Assisted Laryngoscopy and Airway Decontamination Technique on Intubation Quality Metrics in a Helicopter Emergency Medical Service: An Educational Intervention". Air Medical Journal. 39 (2): 107–110. doi:10.1016/j.amj.2019.10.005. ISSN 1067-991X. PMID 32197686. S2CID 209282881. Retrieved 2020-10-25.
- ^ Choi, Insung; Choi, Young Woong; Han, Sang Hyuk; Lee, Ji Heui (2020-12-30). "Successful Endotracheal Intubation Using Suction-Assisted Laryngoscopy Assisted Decontamination Technique and a Head-Down Tilt Position during Massive Regurgitation". Soonchunhyang Medical Science. 26 (2): 75–79. doi:10.15746/sms.20.019. eISSN 2233-4297. ISSN 2233-4289. S2CID 234409328.
- ^ Frantz, Eric; Sarani, Nima; Pirotte, Andrew; Jackson, Bradley S. (2021-01-14). "Woman in respiratory distress". JACEP Open. 2 (1): –12344. doi:10.1002/emp2.12344. ISSN 2688-1152. PMC 7812449. PMID 33490996.