In physiology, dehydration is a lack of total body water that disrupts metabolic processes.[3] It occurs when free water loss exceeds free water intake. This is usually due to excessive sweating, disease, or a lack of access to water. Mild dehydration can also be caused by immersion diuresis, which may increase risk of decompression sickness in divers.
| Dehydration | |
|---|---|
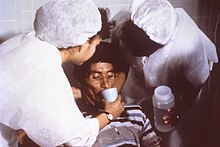 | |
| Nurses encourage a patient to drink an oral rehydration solution to treat dehydration caused by cholera. | |
| Specialty | Critical care medicine |
| Symptoms | Increased thirst, tiredness, decreased urine, dizziness, headaches, and confusion[1] |
| Complications | Low blood volume shock (hypovolemic shock), coma, seizures, urinary tract infection, kidney disease, heatstroke, hypernatremia, metabolic disease,[1] hypertension[2] |
| Causes | Loss of body water |
| Risk factors | Physical water scarcity, heatwaves, disease (most commonly from diseases that cause vomiting and/or diarrhea), exercise |
| Treatment | Drinking clean water |
| Medication | Saline |
Most people can tolerate a 3-4% decrease in total body water without difficulty or adverse health effects. A 5-8% decrease can cause fatigue and dizziness. Loss of over 10% of total body water can cause physical and mental deterioration, accompanied by severe thirst. Death occurs with a 15 and 25% loss of body water.[4] Mild dehydration usually resolves with oral rehydration, but severe cases may need intravenous fluids.
Dehydration can cause hypernatremia (high levels of sodium ions in the blood). This is distinct from hypovolemia (loss of blood volume, particularly blood plasma).
Chronic dehydration can cause kidney stones as well as the development of chronic kidney disease.[5][6]
Signs and symptoms
editThe hallmarks of dehydration include thirst and neurological changes such as headaches, general discomfort, loss of appetite, nausea, decreased urine volume (unless polyuria is the cause of dehydration), confusion, unexplained tiredness, purple fingernails, and seizures.[8] The symptoms of dehydration become increasingly severe with greater total body water loss. A body water loss of 1-2%, considered mild dehydration, is shown to impair cognitive performance.[9] While in people over age 50, the body's thirst sensation diminishes with age, a study found that there was no difference in fluid intake between young and old people.[10] Many older people have symptoms of dehydration, with the most common being fatigue.[11] Dehydration contributes to morbidity in the elderly population, especially during conditions that promote insensible free water losses, such as hot weather.
Cause
editRisk factors for dehydration include but are not limited to: exerting oneself in hot and humid weather, habitation at high altitudes, endurance athletics, elderly adults, infants, children and people living with chronic illnesses.[12][13][14][15]
Dehydration can also come as a side effect from many different types of drugs and medications.[16]
In the elderly, blunted response to thirst or inadequate ability to access free water in the face of excess free water losses (especially hyperglycemia related) seem to be the main causes of dehydration.[17] Excess free water or hypotonic water can leave the body in two ways – sensible loss such as osmotic diuresis, sweating, vomiting and diarrhea, and insensible water loss, occurring mainly through the skin and respiratory tract. In humans, dehydration can be caused by a wide range of diseases and states that impair water homeostasis in the body. These occur primarily through either impaired thirst/water access or sodium excess.[18]
Mechanism
editWater makes up approximately 60% of the human body by mass.[20] Within the body, water is classified as intracellular fluid or extracellular fluid. Intracellular fluid refers to water that is contained within the cells. This consists of approximately 40% of the total body water. Fluid inside the cells has high concentrations of potassium, magnesium, phosphate, and proteins.[21] Extracellular fluid consists of all fluid outside of the cells, and it includes blood and interstitial fluid. This makes up approximately 60% of the total body water. The most common ions in extracellular fluid include sodium, chloride, and bicarbonate.
The concentration of dissolved molecules and ions in the fluid is described as Osmolarity and is measured in osmoles per liter (Osm/L).[21] When the body experiences a free water deficit, the concentration of solutes is increased. This leads to a higher serum osmolarity. When serum osmolarity is elevated, this is detected by osmoreceptors in the hypothalamus. These receptors trigger the release of antidiuretic hormone (ADH).[22] ADH resists dehydration by increasing water absorption in the kidneys and constricting blood vessels. It acts on the V2 receptors in the cells of the collecting tubule of the nephron to increase expression of aquaporin. In more extreme cases of low blood pressure, the hypothalamus releases higher amounts of ADH which also acts on V1 receptors.[23] These receptors cause contractions in the peripheral vascular smooth muscle. This increases systemic vascular resistance and raises blood pressure.
Diagnosis
editDefinition
editDehydration occurs when water intake does not replace free water lost due to normal physiologic processes, including breathing, urination, perspiration, or other causes, including diarrhea, and vomiting. Dehydration can be life-threatening when severe and lead to seizures or respiratory arrest, and also carries the risk of osmotic cerebral edema if rehydration is overly rapid.[24]
The term "dehydration" has sometimes been used incorrectly as a proxy for the separate, related condition of hypovolemia, which specifically refers to a decrease in volume of blood plasma.[3] The two are regulated through independent mechanisms in humans;[3] the distinction is important in guiding treatment.[25]
Physical examination
editCommon exam findings of dehydration include dry mucous membranes, dry axillae, increased capillary refill time, sunken eyes, and poor skin turgor.[27][11] More extreme cases of dehydration can lead to orthostatic hypotension, dizziness, weakness, and altered mental status.[28] Depending on the underlying cause of dehydration, other symptoms may be present as well. Excessive sweating from exercise may be associated with muscle cramps. Patients with gastrointestinal water loss from vomiting or diarrhea may also have fever or other systemic signs of infection.
The skin turgor test can be used to support the diagnosis of dehydration. The skin turgor test is conducted by pinching skin on the patient's body, in a location such as the forearm or the back of the hand, and watching to see how quickly it returns to its normal position. The skin turgor test can be unreliable in patients who have reduced skin elasticity, such as the elderly.[29]
Laboratory tests
editWhile there is no single gold standard test to diagnose dehydration, evidence can be seen in multiple laboratory tests involving blood and urine. Serum osmolarity above 295 mOsm/kg is typically seen in dehydration due to free water loss.[11] A urinalysis, which is a test that performs chemical and microscopic analysis of urine, may find darker color or foul odor with severe dehydration.[30] Urinary sodium also provides information about the type of dehydration. For hyponatremic dehydration, such as from vomiting or diarrhea, urinary sodium will be less than 10mmol/L due to increased sodium retention by the kidneys in an effort to conserve water.[31] In dehydrated patients with sodium loss due to diuretics or renal dysfunction, urinary sodium may be elevated above 20 mmol/L.[32] Patients may also have elevated serum levels of blood urea nitrogen (BUN) and creatinine. Both of these molecules are normally excreted by the kidney, but when the circulating blood volume is low, the kidney can become injured. [33] This causes decreased kidney function and results in elevated BUN and creatinine in the serum.[34]
Prevention
editFor routine activities, thirst is normally an adequate guide to maintain proper hydration.[35] Minimum water intake will vary individually depending on weight, energy expenditure, age, sex, physical activity, environment, diet, and genetics.[36][37] With exercise, exposure to hot environments, or a decreased thirst response, additional water may be required. In athletes in competition, drinking to thirst optimizes performance and safety, despite weight loss, and as of 2010, there was no scientific study showing that it is beneficial to stay ahead of thirst and maintain weight during exercise.[38]
In warm or humid weather, or during heavy exertion, water loss can increase markedly, because humans have a large and widely variable capacity for sweating. Whole-body sweat losses in men can exceed 2 L/h during competitive sport, with rates of 3–4 L/h observed during short-duration, high-intensity exercise in the heat.[39] When such large amounts of water are being lost through perspiration, electrolytes, especially sodium, are also being lost.[40]
In most athletes exercising and sweating for 4–5 hours with a sweat sodium concentration of less than 50 mmol/L, the total sodium lost is less than 10% of total body stores (total stores are approximately 2,500 mmol, or 58 g for a 70-kg person).[41] These losses appear to be well tolerated by most people. The inclusion of sodium in fluid replacement drinks has some theoretical benefits[41] and poses little or no risk, so long as these fluids are hypotonic (since the mainstay of dehydration prevention is the replacement of free water losses).
Treatment
editThe most effective treatment for minor dehydration is widely considered to be drinking water and reducing fluid loss. Plain water restores only the volume of the blood plasma, inhibiting the thirst mechanism before solute levels can be replenished.[42] Consumption of solid foods can also contribute to hydration. It is estimated approximately 22% of American water intake comes from food.[43] Urine concentration and frequency will return to normal as dehydration resolves.[44]
In some cases, correction of a dehydrated state is accomplished by the replenishment of necessary water and electrolytes (through oral rehydration therapy, or fluid replacement by intravenous therapy). As oral rehydration is less painful, non-invasive, inexpensive, and easier to provide, it is the treatment of choice for mild dehydration.[45] Solutions used for intravenous rehydration may be isotonic,hypertonic, or hypotonic depending on the cause of dehydration as well as the sodium concentration in the blood.[46] Pure water injected into the veins will cause the breakdown (lysis) of red blood cells (erythrocytes).[47]
When fresh water is unavailable (e.g. at sea or in a desert), seawater or drinks with significant alcohol concentration will worsen dehydration. Urine contains a lower solute concentration than seawater; this requires the kidneys to create more urine to remove the excess salt, causing more water to be lost than was consumed from seawater.[48] If a person is dehydrated and taken to a medical facility, IVs can also be used.[49]
For severe cases of dehydration where fainting, unconsciousness, or other severely inhibiting symptoms are present (the patient is incapable of standing upright or thinking clearly), emergency attention is required. Fluids containing a proper balance of replacement electrolytes are given orally or intravenously with continuing assessment of electrolyte status; complete resolution is normal in all but the most extreme cases.[50]
Prognosis
editThe prognosis for dehydration depends on the cause and extent of dehydration. Mild dehydration normally resolves with oral hydration. Chronic dehydration, such as from physically demanding jobs or decreased thirst, can lead to chronic kidney disease.[51] Elderly people with dehydration are at higher risk of confusion, urinary tract infections, falls, and even delayed wound healing.[52] In children with mild to moderate dehydration, oral hydration is adequate for a full recovery.[53]
See also
editReferences
edit- ^ a b "Dehydration - Symptoms and causes". Mayo Clinic.
- ^ El-Sharkawy AM, Sahota O, Lobo DN (September 2015). "Acute and chronic effects of hydration status on health". Nutrition Reviews. 73 (Suppl 2): 97–109. doi:10.1093/nutrit/nuv038. PMID 26290295.
- ^ a b c Mange K, Matsuura D, Cizman B, Soto H, Ziyadeh FN, Goldfarb S, et al. (November 1997). "Language guiding therapy: the case of dehydration versus volume depletion". Annals of Internal Medicine. 127 (9): 848–853. doi:10.7326/0003-4819-127-9-199711010-00020. PMID 9382413. S2CID 29854540.
- ^ Ashcroft F, Life Without Water in Life at the Extremes. Berkeley and Los Angeles, 2000, 134-138.
- ^ Seal AD, Suh HG, Jansen LT, Summers LG, Kavouras SA (2019). "Hydration and Health". In Pounis G (ed.). Analysis in Nutrition Research. Elsevier. pp. 299–319. doi:10.1016/b978-0-12-814556-2.00011-7. ISBN 978-0-12-814556-2.
- ^ Clark WF, Sontrop JM, Huang SH, Moist L, Bouby N, Bankir L (2016). "Hydration and Chronic Kidney Disease Progression: A Critical Review of the Evidence". American Journal of Nephrology. 43 (4): 281–292. doi:10.1159/000445959. PMID 27161565.
- ^ "Urine colour chart". Healthdirect Australia. January 2024.
- ^ The Handbook Of The SAS And Elite Forces. How The Professionals Fight And Win. Edited by Jon E. Lewis. p.426-Tactics And Techniques, Survival. Robinson Publishing Ltd 1997. ISBN 1-85487-675-9
- ^ Riebl SK, Davy BM (November 2013). "The Hydration Equation: Update on Water Balance and Cognitive Performance". ACSM's Health & Fitness Journal. 17 (6): 21–28. doi:10.1249/FIT.0b013e3182a9570f. PMC 4207053. PMID 25346594.
- ^ Hall H (August 17, 2020). "Are You Dehydrated?". Skeptical Inquirer. 4 (4).
- ^ a b c Hooper L, Abdelhamid A, Attreed NJ, Campbell WW, Channell AM, Chassagne P, et al. (Cochrane Kidney and Transplant Group) (April 2015). "Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people". The Cochrane Database of Systematic Reviews. 2015 (4): CD009647. doi:10.1002/14651858.CD009647.pub2. hdl:2066/110560. PMC 7097739. PMID 25924806.
- ^ Paulis SJ, Everink IH, Halfens RJ, Lohrmann C, Schols JM (August 1, 2018). "Prevalence and Risk Factors of Dehydration Among Nursing Home Residents: A Systematic Review". Journal of the American Medical Directors Association. 19 (8): 646–657. doi:10.1016/j.jamda.2018.05.009. ISSN 1525-8610. PMID 30056949.
- ^ Sawka MN, Montain SJ (August 1, 2000). "Fluid and electrolyte supplementation for exercise heat stress1234". The American Journal of Clinical Nutrition. NIH Workshop on the Role of Dietary Supplements for Physically Active People. 72 (2): 564S–572S. doi:10.1093/ajcn/72.2.564S. ISSN 0002-9165.
- ^ Steiner MJ, DeWalt DA, Byerley JS (June 9, 2004). "Is This Child Dehydrated?". JAMA. 291 (22): 2746–2754. doi:10.1001/jama.291.22.2746. ISSN 0098-7484. PMID 15187057.
- ^ Research Io, Marriott BM, Carlson SJ (1996), "Fluid Metabolism at High Altitudes", Nutritional Needs In Cold And In High-Altitude Environments: Applications for Military Personnel in Field Operations, National Academies Press (US), retrieved November 15, 2024
- ^ Puga AM, Lopez-Oliva S, Trives C, Partearroyo T, Varela-Moreiras G (March 20, 2019). "Effects of Drugs and Excipients on Hydration Status". Nutrients. 11 (3): 669. doi:10.3390/nu11030669. ISSN 2072-6643. PMC 6470661. PMID 30897748.
- ^ Borra SI, Beredo R, Kleinfeld M (March 1995). "Hypernatremia in the aging: causes, manifestations, and outcome". Journal of the National Medical Association. 87 (3): 220–224. PMC 2607819. PMID 7731073.
- ^ Lindner G, Funk GC (April 2013). "Hypernatremia in critically ill patients". Journal of Critical Care. 28 (2): 216.e11–216.e20. doi:10.1016/j.jcrc.2012.05.001. PMID 22762930.
- ^ Sved A, Walsh D. "Fluid composition of the body 1.3".
- ^ Kamel KS, Halperin ML (2017). Fluid, electrolyte, and acid-base physiology: a problem-based approach (Fifth ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-35515-5.
- ^ a b Garden J, Parks R, Wigmore S (2023). Principles and Practice of Surgery (8th ed.). Elsevier Limited. pp. 32–55. ISBN 978-0-7020-8251-1.
- ^ White BA, Harrison JR, Mehlmann LM (2019). Endocrine and reproductive physiology. Mosby physiology series (5th ed.). St. Louis, MI: Elsevier. ISBN 978-0-323-59573-5.
- ^ Webb AJ, Seisa MO, Nayfeh T, Wieruszewski PM, Nei SD, Smischney NJ (December 2020). "Vasopressin in vasoplegic shock: A systematic review". World Journal of Critical Care Medicine. 9 (5): 88–98. doi:10.5492/wjccm.v9.i5.88. PMC 7754532. PMID 33384951.
- ^ Dehydration at eMedicine
- ^ Bhave G, Neilson EG (August 2011). "Volume depletion versus dehydration: how understanding the difference can guide therapy". American Journal of Kidney Diseases. 58 (2): 302–309. doi:10.1053/j.ajkd.2011.02.395. PMC 4096820. PMID 21705120.
- ^ "UOTW#59 - Ultrasound of the Week". Ultrasound of the Week. September 23, 2015. Retrieved May 27, 2017.
- ^ Huffman GB (September 15, 1999). "Establishing a Bedside Diagnosis of Hypovolemia". American Family Physician. 60 (4): 1220–1225.
- ^ Braun MM, Barstow CH, Pyzocha NJ (March 1, 2015). "Diagnosis and Management of Sodium Disorders: Hyponatremia and Hypernatremia". American Family Physician. 91 (5): 299–307. PMID 25822386.
- ^ Thomas J, Monaghan T (2014). Oxford Handbook of Clinical Examination and Practical Skills. Oxford University Press. ISBN 978-0-19-959397-2.
- ^ Hughes G (2021). A medication guide to internal medicine tests and procedures (First ed.). Philadelphia: Elsevier, Inc. ISBN 978-0-323-79007-9.
- ^ Tietze KJ (2012), "Review of Laboratory and Diagnostic Tests", Clinical Skills for Pharmacists, Elsevier, pp. 86–122, doi:10.1016/b978-0-323-07738-5.10005-5, ISBN 978-0-323-07738-5, retrieved November 6, 2024
- ^ Yun G, Baek SH, Kim S (May 1, 2023). "Evaluation and management of hypernatremia in adults: clinical perspectives". The Korean Journal of Internal Medicine. 38 (3): 290–302. doi:10.3904/kjim.2022.346. ISSN 1226-3303. PMC 10175862. PMID 36578134.
- ^ Mohamed MS, Martin A (May 2024). "Acute kidney injury in critical care". Anaesthesia & Intensive Care Medicine. 25 (5): 308–315. doi:10.1016/j.mpaic.2024.03.008.
- ^ Amin R, Ahn SY, Moudgil A (2021), "Kidney and urinary tract disorders", Biochemical and Molecular Basis of Pediatric Disease, Elsevier, pp. 167–228, doi:10.1016/b978-0-12-817962-8.00010-x, ISBN 978-0-12-817962-8, retrieved November 6, 2024
- ^ Institute of Medicine, Food Nutrition Board (June 18, 2005). Dietary Reference Intakes: Water, Potassium, Sodium, Chloride, and Sulfate : Health and Medicine Division. National Academies Press. ISBN 9780309091695. Retrieved February 7, 2018.
- ^ Armstrong LE, Johnson EC (December 5, 2018). "Water Intake, Water Balance, and the Elusive Daily Water Requirement". Nutrients. 10 (12): 1928. doi:10.3390/nu10121928. ISSN 2072-6643. PMC 6315424. PMID 30563134.
- ^ Yamada Y, Zhang X, Henderson ME, Sagayama H, Pontzer H, Watanabe D, et al. (November 2022). "Variation in human water turnover associated with environmental and lifestyle factors". Science. 378 (6622): 909–915. Bibcode:2022Sci...378..909I. doi:10.1126/science.abm8668. PMC 9764345. PMID 36423296.
- ^ Noakes TD (2010). "Is drinking to thirst optimum?". Annals of Nutrition & Metabolism. 57 (Suppl 2): 9–17. doi:10.1159/000322697. PMID 21346332.
- ^ Taylor NA, Machado-Moreira CA (February 2013). "Regional variations in transepidermal water loss, eccrine sweat gland density, sweat secretion rates and electrolyte composition in resting and exercising humans". Extreme Physiology & Medicine. 2 (1): 4. doi:10.1186/2046-7648-2-4. PMC 3710196. PMID 23849497.
- ^ Baker LB (March 2017). "Sweating Rate and Sweat Sodium Concentration in Athletes: A Review of Methodology and Intra/Interindividual Variability". Sports Medicine. 47 (S1): 111–128. doi:10.1007/s40279-017-0691-5. ISSN 0112-1642. PMC 5371639. PMID 28332116.
- ^ a b Coyle EF (January 2004). "Fluid and fuel intake during exercise". Journal of Sports Sciences. 22 (1): 39–55. CiteSeerX 10.1.1.321.6991. doi:10.1080/0264041031000140545. PMID 14971432. S2CID 14693195.
- ^ Murray R, Stofan J (2001). "Ch. 8: Formulating carbohydrate-electrolyte drinks for optimal efficacy". In Maughan RJ, Murray R (eds.). Sports Drinks: Basic Science and Practical Aspects. CRC Press. pp. 197–224. ISBN 978-0-8493-7008-3.
- ^ Popkin BM, D'Anci KE, Rosenberg IH (August 2010). "Water, hydration, and health: Nutrition Reviews©, Vol. 68, No. 8". Nutrition Reviews. 68 (8): 439–458. doi:10.1111/j.1753-4887.2010.00304.x. PMC 2908954. PMID 20646222.
- ^ Ostermann M, Shaw AD, Joannidis M (January 1, 2023). "Management of oliguria". Intensive Care Medicine. 49 (1): 103–106. doi:10.1007/s00134-022-06909-5. ISSN 1432-1238. PMID 36266588.
- ^ Aghsaeifard Z, Heidari G, Alizadeh R (September 2022). "Understanding the use of oral rehydration therapy: A narrative review from clinical practice to main recommendations". Health Science Reports. 5 (5): e827. doi:10.1002/hsr2.827. ISSN 2398-8835. PMC 9464461. PMID 36110343.
- ^ Kim SW (2006). "Hypernatemia : Successful Treatment". Electrolyte & Blood Pressure. 4 (2): 66–71. doi:10.5049/EBP.2006.4.2.66. ISSN 1738-5997. PMC 3894528. PMID 24459489.
- ^ Tinawi M (April 21, 2021). "New Trends in the Utilization of Intravenous Fluids". Cureus. 13 (4): e14619. doi:10.7759/cureus.14619. ISSN 2168-8184. PMC 8140055. PMID 34040918.
- ^ Hall JE, Hall ME, Guyton AC (2021). Guyton and Hall textbook of medical physiology (14th ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-67280-1.
- ^ Gawronska J, Koyanagi A, López Sánchez GF, Veronese N, Ilie PC, Carrie A, et al. (December 31, 2022). "The Prevalence and Indications of Intravenous Rehydration Therapy in Hospital Settings: A Systematic Review". Epidemiologia. 4 (1): 18–32. doi:10.3390/epidemiologia4010002. ISSN 2673-3986. PMC 9844368. PMID 36648776.
- ^ Ellershaw JE, Sutcliffe JM, Saunders CM (April 1995). "Dehydration and the dying patient". Journal of Pain and Symptom Management. 10 (3): 192–197. doi:10.1016/0885-3924(94)00123-3. PMID 7629413.
- ^ El Khayat M, Halwani DA, Hneiny L, Alameddine I, Haidar MA, Habib RR (February 8, 2022). "Impacts of Climate Change and Heat Stress on Farmworkers' Health: A Scoping Review". Frontiers in Public Health. 10. doi:10.3389/fpubh.2022.782811. ISSN 2296-2565. PMC 8861180. PMID 35211437.
- ^ Bruno C, Collier A, Holyday M, Lambert K (October 18, 2021). "Interventions to Improve Hydration in Older Adults: A Systematic Review and Meta-Analysis". Nutrients. 13 (10): 3640. doi:10.3390/nu13103640. ISSN 2072-6643. PMC 8537864. PMID 34684642.
- ^ Canavan A, Billy S Arant J (October 1, 2009). "Diagnosis and Management of Dehydration in Children". American Family Physician. 80 (7): 692–696. PMID 19817339.
Further reading
edit- Byock I (1995). "Patient refusal of nutrition and hydration: walking the ever-finer line". The American Journal of Hospice & Palliative Care. 12 (2): 8, 9–8, 13. doi:10.1177/104990919501200205. PMID 7605733. S2CID 46385519.
- Steiner MJ, DeWalt DA, Byerley JS (June 2004). "Is this child dehydrated?". JAMA. 291 (22): 2746–2754. doi:10.1001/jama.291.22.2746. PMID 15187057.