This article may need to be rewritten to comply with Wikipedia's quality standards. (January 2018) |
Ira Robert Byock (/ˈbaɪɒk/ BYE-ok;[4] born February 13, 1951, Newark, New Jersey) is an American physician, author, and advocate for palliative care. He is founder and chief medical officer of the Providence St. Joseph Health Institute for Human Caring in Torrance, California, and holds appointments as active emeritus professor of medicine and professor of community health and family medicine at the Geisel School of Medicine at Dartmouth College. He was director of palliative medicine at Dartmouth–Hitchcock Medical Center, from 2003–14, and associate director for patient and family-centered care at the affiliated Norris-Cotton Cancer Center.
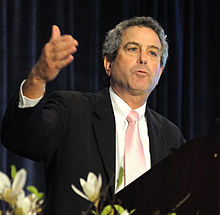
Ira Byock | |
|---|---|
 | |
| Born | February 13, 1951 Newark, New Jersey, United States |
| Nationality | American |
| Occupation | Physician |
| Known for | Author, advocate for palliative care |
| Title |
|
| Honors | Fellow of the American Academy of Hospice and Palliative Medicine[3] |
| Website | irabyock |
Byock's early career focused on emergency medicine and rural practice in parallel with an interest in hospice care, and then founded the Missoula Demonstration Project and became director for the Robert Wood Johnson Promoting Excellence in End-of-Life Care initiative. His books include Dying Well (1997), The Four Things That Matter Most (2004), and The Best Care Possible (2012).
Education and medical training
editByock earned a bachelor's degree in biology from the University of Colorado, Boulder, in 1973, and Doctor of Medicine from the University of Colorado School of Medicine-Denver in 1978. He completed an internship and residency in family practice medicine in University of California–San Francisco in Fresno Archived 2017-07-09 at the Wayback Machine, California (1978–81).[citation needed]
He holds certifications from the American Board of Family Practice (since 1981), the American Board of Hospice and Palliative Medicine (since 1996), and the American Board of Emergency Medicine (1989–1998). He is also a Fellow of the American Academy of Family Medicine (since 1986) and the American Academy of Hospice and Palliative Medicine.[3]
Career and professional focus
editThis section of a biography of a living person needs additional citations for verification. (January 2018) |
While Byock's early career focus was on rural family practice and emergency medicine,[5] he developed an interest in the then-nascent hospice movement. While still an intern in 1978–79, Byock teamed with a social work intern to create the Esperanza Care Cooperative, a “fledgling hospice program” for Valley Medical Center in California's Central Valley.[5]
From 1982–96 as an emergency physician, mainly in rural and small city settings in Montana, Byock maintained an interest in end-of-life care. In particular, he was interested in exploring, measuring, and developing therapeutic supports for the entirety of a person's experience of suffering, dying, and in well-being.[5] Along with Melanie Merriman, Byock developed the Missoula-VITAS Quality of Life Index, a clinical assessment tool designed to measure subjective quality of life in persons with serious illness. The index was intended to fill a gap in clinical assessment tools, which at the time were mostly focused on physiological indicators or observable function, rather than on subjective evaluations of well-being and suffering. An insight derived from the tool's use is that subjective well-being may exist even in the presence of severe functional impairment and high symptom burden.[6]
While among the best-rated instruments in terms of validity,[7] including cross-cultural,[8] the Missoula-VITAS Quality of Life Index is considered better in clinical applications, as a psychometric as well as therapeutic tool, than in research.[9]
In 1996, Byock was asked to lead the Robert Wood Johnson Foundation's national program in Promoting Excellence in End-of-Life Care, intended to expand access to hospice and palliative care to regions and populations not easily served under the Medicare Hospice Benefit. Under Byock's leadership with deputy director, Jeanne Shields Twohig, the program directed up to $15 million over 10 years to 26 demonstration projects to develop and test models for palliative care within a variety of medical specialties, care settings, and underserved populations. Eight peer workgroups of healthcare leaders specifically focused on specific diseases or issues, while nine projects addressed knowledge and practice gaps—all under an overarching communications strategy, with significant results.[10]
Also in 1996, with separate funding from another program area of the Robert Wood Johnson Foundation, Byock co-founded (with Barbara Spring, PhD) and served as principal investigator for the Missoula Demonstration Project, a community organization focused on studying the experiences of illness, dying, caregiving, and grieving within the context of community, and engaging the community of Missoula, Montana in improving care and support for seriously ill people and their families.[11]
During the 1990s, Byock helped to launch and assumed leadership roles in the American Academy of Hospice and Palliative Medicine[5] serving on the Ethics Committee (1990–96), the Board of Directors (1990–96), as organizational secretary (1995), and as president (1997). From 1998 to 2002, he served as founding member and member of the Board of Directors and Executive Committee of the Partnership for Caring, which later became the Last Acts Partnership, also funded by the Robert Wood Johnson Foundation (RWJF).[12] During this period, Byock had a faculty appointment at the University of Montana, Practical Ethics Center, as research professor of philosophy.[citation needed]
In late 2003, Byock moved to New Hampshire as director of palliative medicine for Dartmouth-Hitchcock Medical Center and associate director for patient and family-centered care at the affiliated Norris-Cotton Cancer Center. He remains an active emeritus professor of medicine and of community health and family medicine at Dartmouth's Geisel School of Medicine.[2]
In 2014, he founded the Institute for Human Caring of Providence Health & Services in Torrance, California, where he currently serves as chief medical officer.[1]
Opposition to physician-assisted suicide
editByock has been critical of right to die movements, physician-assisted suicide, the Oregon Death with Dignity Act, and the California End of Life Option Act.[13]
Interviews and media appearances
editByock has appeared as a featured guest on national television and radio programs, including NPR's Talk of the Nation,[14][15][16][17] All Things Considered,[18][19][20] Fresh Air,[21] American Public Media's On Being,[22] CBS's 60 Minutes,[23][24] ABC News Nightline,[25] and PBS NewsHour.[26][27][28]
Personal life
editByock is married to Yvonne Corbeil[29] who is a nurse and currently serves as Senior Advisor for the Institute for Human Caring, Providence St. Joseph Health and Co-Director, Clinical Transformation Specialists.
Publications
editBooks
edit- The Best Care Possible: A physician’s quest to transform care through the end of life. New York: Avery, 2012.
- Dying well: The prospect for growth at the end of life. New York: Riverhead/Putnam Books, 1997.
- The Four Things That Matter Most: A book about living (2nd ed.). New York: Atria Books, a division of Simon and Schuster, 2014.
- The Four Things That Matter Most: A book about living. New York: Free Press, a division of Simon and Schuster, 2004.
- Heffner J. & I. Byock (eds). Palliative and end of life pearls. Philadelphia, PA: Hanley & Belfus, 2002.
- Staton J, Shuy R, Byock I. A few months to live: Different paths to life's end. Washington, DC: Georgetown University Press, 2001.
References
edit- ^ a b "Our Team | The Institute for Human Caring | Providence St. Joseph Health". Institute for Human Caring. Retrieved May 15, 2020.
- ^ a b "Ira R. Byock, MD – Faculty Expertise Database – Geisel School of Medicine at Dartmouth". Retrieved May 15, 2020.
- ^ a b "Fellows of the American Academy of Hospice and Palliative Medicine | AAHPM". American Academy of Hospice and Palliative Medicine. Retrieved May 15, 2020.
- ^ "You've Got Dr. Ira Byock". Archived from the original on 2021-12-21. Retrieved 5 September 2020.
- ^ a b c d Byock, I. (2009). "Suffering and wellness". Journal of Palliative Medicine. 12 (9): 785–7. doi:10.1089/jpm.2009.9568. PMID 19719371.
- ^ Byock, I. (2014). Missoula-Vitas Quality-of-Life Index. In Michalos, AC (ed.). Encyclopedia of quality of life and well-being research. Dordrecht, Netherlands: Springer Reference.
- ^ Chang, VT, Weissman, DE. (2015). Quality of life. Fast Facts & Concepts #52. Palliative Care Network of Wisconsin. Retrieved from http://www.mypcnow.org/blank-f8z8n.
- ^ Namisango, E., E. Katabira, C. Karamagi, P. Baguma. (2007). Validation of the Missoula-Vitas Quality-of-Life Index among patients with advanced AIDS in urban Kampala, Uganda, Journal of Pain & Symptom Management, 33(2), 189–202); accessed January 5, 2018.
- ^ Schwartz, CE, Merriman, MP, Reed, G, & Byock, I. (2005). Evaluation of the Missoula-VITAS Quality of Life Index--revised: research tool or clinical tool? Journal of Palliative Medicine, 8(1), 121–35.
- ^ Promoting excellence in end-of-life care, Robert Wood Johnson Foundation (2009)
- ^ Crum, R. (2005, March 25). Missoula, Montana project studies a community's perspective on death and dying to improve end-of-life care, rwjf.org; accessed January 5, 2018.
- ^ National Hospice & Palliative Care Organization (NHPCO), http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3402.
- ^ Ira Byock, "We should think twice about 'death with dignity'", Los Angeles Times, January 30, 2015.
- ^ "Physician-Assisted Suicide Debate". NPR. March 10, 1997.
- ^ "End-Of-Life Care". NPR. August 15, 1997.
- ^ "Making Plans For The Last Chapter Of Life". NPR. August 31, 2009.
- ^ "'Best Care': We Make Death Harder Than It Has To Be". NPR. March 26, 2012.
- ^ "Scotus: Doctor Assisted Suicide". NPR. June 26, 1997.
- ^ "Dying Well In Montana". NPR. November 6, 1997.
- ^ "Hopes, Fears At Vermont Health Care Forum". NPR. March 17, 2009.
- ^ "Dr. IRA BYOCK talks about his new book "Dying Well: The Prospect of Growth at the End of Life". NPR. February 10, 1997.
- ^ "Ira Byock — Contemplating Mortality | On Being". On Being. December 1, 2015. Archived from the original on December 1, 2015.
- ^ "The Cost of Dying". CBS News. November 9, 2009.
- ^ "A doctor reflects on death and dignity". CBS News. October 19, 2014.
- ^ "Video: Living Better Means Living Longer". ABC News. August 18, 2010.
- ^ "Video". PBS NewsHour. October 14, 2014. Archived from the original on August 8, 2014.
- ^ "Should terminally ill patients be able to choose when they die?". PBS NewsHour. October 14, 2014.
- ^ "New guidelines may encourage end-of-life discussions". PBS NewsHour. August 8, 2015.
- ^ Stephenson Carter, Laura. "End-of-life expert Ira Byock will lead palliative care unit". Dartmouth.edu. Vital Signs. Retrieved 30 June 2019.
External links
edit- Profile, IraByock.org
- The Four Things That Matter Most, WikiSummaries.org