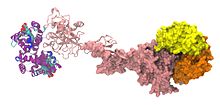
Haptoglobin (abbreviated as Hp) is the protein that in humans is encoded by the HP gene.[5][6] In blood plasma, haptoglobin binds with high affinity to free hemoglobin[7] released from erythrocytes, and thereby inhibits its deleterious oxidative activity. Compared to Hp, hemopexin binds to free heme.[8] The haptoglobin-hemoglobin complex will then be removed by the reticuloendothelial system (mostly the spleen).
In clinical settings, the haptoglobin assay is used to screen for and monitor intravascular hemolytic anemia. In intravascular hemolysis, free hemoglobin will be released into circulation and hence haptoglobin will bind the hemoglobin. This causes a decline in haptoglobin levels.
The protein was discovered as a "plasma substance" in 1938 by French biochemists Max-Fernand Jayle and Michel Polonovski.[9][10]
Function
editHemoglobin that has been released into the blood plasma by damaged red blood cells has harmful effects. The HP gene encodes a preproprotein that is processed to yield both alpha and beta chains, which subsequently combines as a tetramer to produce haptoglobin. Haptoglobin functions to bind the free plasma hemoglobin, which allows degradative enzymes to gain access to the hemoglobin while at the same time preventing loss of iron through the kidneys and protecting the kidneys from damage by hemoglobin.[11]
The cellular receptor target of Hp is the monocyte/macrophage scavenger receptor, CD163.[7] Following Hb-Hp binding to CD163, cellular internalization of the complex leads to globin and heme metabolism, which is followed by adaptive changes in antioxidant and iron metabolism pathways and macrophage phenotype polarization.[7]
Hp has hemoglobin-independent immunomodulatory functions. It dampens lipopolysaccharide-induced cytokine expression.[12] Lipopolysaccharides directly bind to Hp, which, due to the high abundance of Hp in serum, results in their buffering and shielding from toll-like receptor 4. Functionally, this results in delayed activation of the NF-κB pathway.[13]
Difference from hemopexin
editWhen hemoglobin is released from RBCs within the physiologic range of haptoglobin, the potential deleterious effects of hemoglobin are prevented. During hyper-hemolytic conditions or with chronic hemolysis, haptoglobin is depleted and hemoglobin readily distributes to tissues where it might be exposed to oxidative conditions. In such conditions, heme can be released from ferric (Fe3+-bound) hemoglobin. The free heme can then accelerate tissue damage by promoting peroxidative reactions and activation of inflammatory cascades. Hemopexin (Hx) is another plasma glycoprotein that is able to bind heme with high affinity. It sequesters heme in an inert non-toxic form and transports it to the liver for catabolism and excretion.[7]
Synthesis
editHaptoglobin is produced mostly by hepatic cells but also by other tissues such as skin, lung and kidney. In addition, the haptoglobin gene is expressed in murine and human adipose tissue.[14]
Haptoglobin had been shown to be expressed in adipose tissue of cattle as well.[15]
Structure
editHaptoglobin, in its simplest form, consists of two alpha and two beta chains, connected by disulfide bridges. The chains originate from a common precursor protein, which is proteolytically cleaved during protein synthesis.
Hp exists in two allelic forms in the human population, so-called Hp1 and Hp2, the latter one having arisen due to the partial duplication of Hp1 gene. Three genotypes of Hp, therefore, are found in humans: Hp1-1, Hp2-1, and Hp2-2. Hp of different genotypes have been shown to bind hemoglobin with different affinities, with Hp2-2 being the weakest binder. Allele 2 encodes for two multimerization domains. This results in oligomer formation in carriers of allele 2.[5] The frequency of the short allele varies between 7% and 70% depending on racial origin.[16] It is unclear which evolutionary advantage is conferred by the longer allele; strikingly, a similar partial duplication independently arose much earlier in a precursor of ruminants. Ruminants exclusively express oligomeric haptoglobin.[17]
In other species
editHp has been found in all mammals studied so far, some birds, e.g., cormorant and ostrich but also, in its simpler form, in bony fish, e.g., zebrafish. Hp is absent in at least some amphibians (Xenopus) and neognathous birds (chicken and goose).
Clinical significance
editMutations in this gene or its regulatory regions cause ahaptoglobinemia or hypohaptoglobinemia. This gene has also been linked to diabetic nephropathy,[18] the incidence of coronary artery disease in type 1 diabetes,[19] Crohn's disease,[20] inflammatory disease behavior, primary sclerosing cholangitis, susceptibility to idiopathic Parkinson's disease,[21] and a reduced incidence of Plasmodium falciparum malaria.[22]
Since the reticuloendothelial system will remove the haptoglobin-hemoglobin complex from the body,[8] haptoglobin levels will be decreased in case of intravascular hemolysis or severe extravascular hemolysis. In the process of binding to free hemoglobin, haptoglobin sequesters the iron within hemoglobin, preventing iron-utilizing bacteria from benefiting from hemolysis. It is theorized that, because of this, haptoglobin has evolved into an acute-phase protein. HP has a protective influence on the hemolytic kidney.[23][24]
The different haptoglobin phenotypes differ in their antioxidant, scavenging,[25] and immunomodulatory properties. This aspect of haptoglobin may gain importance in immune suppressed conditions (such as liver cirrhosis) and the various phenotypes may result in different susceptibility levels towards bacterial infections.[26]
Some studies associate certain haptoglobin phenotypes with the risk of developing hypertension in diabetes[27] and schizophrenia.[28]
Test protocol
editMeasuring the level of haptoglobin in a patient's blood is ordered whenever a patient exhibits symptoms of anemia, such as pallor, fatigue, or shortness of breath, along with physical signs of hemolysis, such as jaundice or dark-colored urine. The test is also commonly ordered as a hemolytic anemia battery, which also includes a reticulocyte count and a peripheral blood smear. It can also be ordered along with a direct antiglobulin test when a patient is suspected of having a transfusion reaction or symptoms of autoimmune hemolytic anemia. Also, it may be ordered in conjunction with a bilirubin.
Interpretation
editA decrease in haptoglobin can support a diagnosis of hemolysis, especially when correlated with a decreased hemoglobin, and hematocrit, and also an increased reticulocyte count. Low haptoglobin levels occur regardless of the site and mechanism of haemolysis (intravascular and splenic/"extravascular") [29]
If the reticulocyte count is increased, but the haptoglobin level is normal, this argues against haemolysis, and suggests a bone marrow response to blood loss. If there are symptoms of anemia but both the reticulocyte count and the haptoglobin level are normal, the anemia is most likely not due to hemolysis. Haptoglobin levels that are decreased but do not accompany signs of anemia may indicate advanced liver damage, as the liver is the major site of production of haptoglobin.
As haptoglobin is an acute-phase protein, any inflammatory process (infection, injury, allergy, etc.) may increase the levels of plasma haptoglobin, but patients with haemolysis usually have low haptoglobin regardless of the presence of inflammation [30]
See also
editReferences
edit- This article incorporates text from the United States National Library of Medicine, which is in the public domain.
- ^ a b c GRCh38: Ensembl release 89: ENSG00000257017 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000031722 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Dobryszycka W (September 1997). "Biological functions of haptoglobin--new pieces to an old puzzle". European Journal of Clinical Chemistry and Clinical Biochemistry. 35 (9): 647–654. PMID 9352226.
- ^ Wassell J (2000). "Haptoglobin: function and polymorphism". Clinical Laboratory. 46 (11–12): 547–552. PMID 11109501.
- ^ a b c d Schaer DJ, Vinchi F, Ingoglia G, Tolosano E, Buehler PW (28 October 2014). "Haptoglobin, hemopexin, and related defense pathways-basic science, clinical perspectives, and drug development". Frontiers in Physiology. 5. Frontiers Media SA: 415. doi:10.3389/fphys.2014.00415. PMC 4211382. PMID 25389409.
- ^ a b "Intravascular hemolysis". eClinpath. Retrieved 8 May 2019.
- ^ Shih AW, McFarlane A, Verhovsek M (April 2014). "Haptoglobin testing in hemolysis: measurement and interpretation". American Journal of Hematology. 89 (4): 443–447. doi:10.1002/ajh.23623. PMID 24809098.
- ^ "Haptoglobins". New England Journal of Medicine. 266 (11): 569–570. 15 March 1962. doi:10.1056/NEJM196203152661115. ISSN 0028-4793.
- ^ "Entrez Gene: HP".
- ^ Arredouani MS, Kasran A, Vanoirbeek JA, Berger FG, Baumann H, Ceuppens JL (February 2005). "Haptoglobin dampens endotoxin-induced inflammatory effects both in vitro and in vivo". Immunology. 114 (2): 263–271. doi:10.1111/j.1365-2567.2004.02071.x. PMC 1782073. PMID 15667571.
- ^ Zein L, Grossmann J, Swoboda H, Borgel C, Wilke B, Awe S, Nist A, Stiewe T, Stehling O, Freibert SA, Adhikary T, Chung HR (2024). "Haptoglobin buffers lipopolysaccharides to delay activation of NFκB". Frontiers in Immunology. 15. doi:10.3389/fimmu.2024.1401527. PMC 11479958. PMID 39416789.
- ^ Trayhurn P, Wood IS (September 2004). "Adipokines: inflammation and the pleiotropic role of white adipose tissue". The British Journal of Nutrition. 92 (3): 347–355. doi:10.1079/BJN20041213. PMID 15469638.
- ^ Saremi B, Al-Dawood A, Winand S, Müller U, Pappritz J, von Soosten D, et al. (May 2012). "Bovine haptoglobin as an adipokine: serum concentrations and tissue expression in dairy cows receiving a conjugated linoleic acids supplement throughout lactation". Veterinary Immunology and Immunopathology. 146 (3–4): 201–211. doi:10.1016/j.vetimm.2012.03.011. PMID 22498004.
- ^ Carter K, Worwood M (April 2007). "Haptoglobin: a review of the major allele frequencies worldwide and their association with diseases". International Journal of Laboratory Hematology. 29 (2): 92–110. doi:10.1111/j.1751-553X.2007.00898.x. PMID 17474882.
- ^ Wicher KB, Fries E (October 2007). "Convergent evolution of human and bovine haptoglobin: partial duplication of the genes". Journal of Molecular Evolution. 65 (4): 373–379. Bibcode:2007JMolE..65..373W. doi:10.1007/s00239-007-9002-3. PMID 17922076. S2CID 9958602.
- ^ Asleh R, Levy AP (2005). "In vivo and in vitro studies establishing haptoglobin as a major susceptibility gene for diabetic vascular disease". Vascular Health and Risk Management. 1 (1): 19–28. doi:10.2147/vhrm.1.1.19.58930. PMC 1993923. PMID 17319095.
- ^ Sadrzadeh SM, Bozorgmehr J (June 2004). "Haptoglobin phenotypes in health and disorders". American Journal of Clinical Pathology. 121 (Suppl): S97-104. doi:10.1309/8GLX5798Y5XHQ0VW. PMID 15298155.
- ^ Papp M, Lakatos PL, Palatka K, Foldi I, Udvardy M, Harsfalvi J, et al. (May 2007). "Haptoglobin polymorphisms are associated with Crohn's disease, disease behavior, and extraintestinal manifestations in Hungarian patients". Digestive Diseases and Sciences. 52 (5): 1279–1284. doi:10.1007/s10620-006-9615-1. PMID 17357835. S2CID 35999438.
- ^ Costa-Mallen P, Checkoway H, Zabeti A, Edenfield MJ, Swanson PD, Longstreth WT, et al. (March 2008). "The functional polymorphism of the hemoglobin-binding protein haptoglobin influences susceptibility to idiopathic Parkinson's disease". American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics. 147B (2): 216–222. doi:10.1002/ajmg.b.30593. PMID 17918239. S2CID 21568460.
- ^ Prentice AM, Ghattas H, Doherty C, Cox SE (December 2007). "Iron metabolism and malaria". Food and Nutrition Bulletin. 28 (4 Suppl): S524–S539. doi:10.1177/15648265070284S406. PMID 18297891.
- ^ Pintera J (1968). "The protective influence of haptoglobin on hemoglobinuric kidney. I. Bioch- emical and macroscopic observations". Folia Haematologica. 90 (1): 82–91. PMID 4176393.
- ^ Miederer SE, Hotz J (December 1969). "[Pathogenesis of kidney hemolysis]". Bruns' Beiträge für Klinische Chirurgie (in German). 217 (7): 661–665. PMID 5404273.
- ^ Olaniyan OO, Odewusi OO, Osadolor HB (2021). "Oxidative protein modification and chromosomal instability among type 2 diabetics in Osogbo, Nigeria. ". Alexandria Journal of Medicine (TAJM). 57: 168–176. doi:10.1080/20905068.2021.1935123.
- ^ Vitalis Z, Altorjay I, Tornai I, Palatka K, Kacska S, Palyu E, et al. (April 2011). "Phenotypic polymorphism of haptoglobin: a novel risk factor for the development of infection in liver cirrhosis". Human Immunology. 72 (4): 348–354. doi:10.1016/j.humimm.2011.01.008. PMID 21262313.
- ^ Odewusi Odeyinka O, Ogberetitinor Ofejiro B, Ijeh Wendy A, Obadire Olalere S, Olaniyan Olayinka O (July–September 2023). "Evaluation Of Neuronal Inflammation And Oxidative Dna Damage In Different Haptoglobin Phenotypes Of A Nigerian Type-2 Diabetes Population" (PDF). Journal of Krishna Institute of Medical Science University. 12 (3): 50–62.
- ^ Gene Overview of All Published Schizophrenia-Association Studies for HP Archived 21 February 2009 at the Wayback Machine - SzGene database at Schizophrenia Research Forum.
- ^ Körmöczi GF, Säemann MD, Buchta C, Peck-Radosavljevic M, Mayr WR, Schwartz DW, et al. (March 2006). "Influence of clinical factors on the haemolysis marker haptoglobin". European Journal of Clinical Investigation. 36 (3): 202–209. doi:10.1111/j.1365-2362.2006.01617.x. PMID 16506966. S2CID 39884908.
- ^ Körmöczi GF, Säemann MD, Buchta C, Peck-Radosavljevic M, Mayr WR, Schwartz DW, et al. (March 2006). "Influence of clinical factors on the haemolysis marker haptoglobin". European Journal of Clinical Investigation. 36 (3): 202–209. doi:10.1111/j.1365-2362.2006.01617.x. PMID 16506966. S2CID 39884908.
Further reading
edit- Graversen JH, Madsen M, Moestrup SK (April 2002). "CD163: a signal receptor scavenging haptoglobin-hemoglobin complexes from plasma". The International Journal of Biochemistry & Cell Biology. 34 (4): 309–314. doi:10.1016/S1357-2725(01)00144-3. PMID 11854028.
- Madsen M, Graversen JH, Moestrup SK (2002). "Haptoglobin and CD163: captor and receptor gating hemoglobin to macrophage lysosomes". Redox Report. 6 (6): 386–388. doi:10.1179/135100001101536490. PMID 11865982.
- Erickson LM, Kim HS, Maeda N (December 1992). "Junctions between genes in the haptoglobin gene cluster of primates". Genomics. 14 (4): 948–958. doi:10.1016/S0888-7543(05)80116-8. PMID 1478675.
- Maeda N (June 1985). "Nucleotide sequence of the haptoglobin and haptoglobin-related gene pair. The haptoglobin-related gene contains a retrovirus-like element". The Journal of Biological Chemistry. 260 (11): 6698–6709. doi:10.1016/S0021-9258(18)88836-6. PMID 2987228.
- Simmers RN, Stupans I, Sutherland GR (1986). "Localization of the human haptoglobin genes distal to the fragile site at 16q22 using in situ hybridization". Cytogenetics and Cell Genetics. 41 (1): 38–41. doi:10.1159/000132193. PMID 3455911.
- van der Straten A, Falque JC, Loriau R, Bollen A, Cabezón T (April 1986). "Expression of cloned human haptoglobin and alpha 1-antitrypsin complementary DNAs in Saccharomyces cerevisiae". DNA. 5 (2): 129–136. doi:10.1089/dna.1986.5.129. PMID 3519135.
- Bensi G, Raugei G, Klefenz H, Cortese R (January 1985). "Structure and expression of the human haptoglobin locus". The EMBO Journal. 4 (1): 119–126. doi:10.1002/j.1460-2075.1985.tb02325.x. PMC 554159. PMID 4018023.
- Malchy B, Dixon GH (March 1973). "Studies on the interchain disulfides of human haptoglobins". Canadian Journal of Biochemistry. 51 (3): 249–264. doi:10.1139/o73-032. PMID 4573324.
- Raugei G, Bensi G, Colantuoni V, Romano V, Santoro C, Costanzo F, Cortese R (September 1983). "Sequence of human haptoglobin cDNA: evidence that the alpha and beta subunits are coded by the same mRNA". Nucleic Acids Research. 11 (17): 5811–5819. doi:10.1093/nar/11.17.5811. PMC 326319. PMID 6310515.
- Yang F, Brune JL, Baldwin WD, Barnett DR, Bowman BH (October 1983). "Identification and characterization of human haptoglobin cDNA". Proceedings of the National Academy of Sciences of the United States of America. 80 (19): 5875–5879. Bibcode:1983PNAS...80.5875Y. doi:10.1073/pnas.80.19.5875. PMC 390178. PMID 6310599.
- Maeda N, Yang F, Barnett DR, Bowman BH, Smithies O (1984). "Duplication within the haptoglobin Hp2 gene". Nature. 309 (5964): 131–135. Bibcode:1984Natur.309..131M. doi:10.1038/309131a0. PMID 6325933. S2CID 4368535.
- Brune JL, Yang F, Barnett DR, Bowman BH (June 1984). "Evolution of haptoglobin: comparison of complementary DNA encoding Hp alpha 1S and Hp alpha 2FS". Nucleic Acids Research. 12 (11): 4531–4538. doi:10.1093/nar/12.11.4531. PMC 318856. PMID 6330675.
- van der Straten A, Herzog A, Cabezón T, Bollen A (March 1984). "Characterization of human haptoglobin cDNAs coding for alpha 2FS beta and alpha 1S beta variants". FEBS Letters. 168 (1): 103–107. Bibcode:1984FEBSL.168..103V. doi:10.1016/0014-5793(84)80215-X. PMID 6546723. S2CID 85082741.
- vander Straten A, Herzog A, Jacobs P, Cabezón T, Bollen A (1984). "Molecular cloning of human haptoglobin cDNA: evidence for a single mRNA coding for alpha 2 and beta chains". The EMBO Journal. 2 (6): 1003–1007. doi:10.1002/j.1460-2075.1983.tb01534.x. PMC 555221. PMID 6688992.
- Kurosky A, Barnett DR, Lee TH, Touchstone B, Hay RE, Arnott MS, et al. (June 1980). "Covalent structure of human haptoglobin: a serine protease homolog". Proceedings of the National Academy of Sciences of the United States of America. 77 (6): 3388–3392. Bibcode:1980PNAS...77.3388K. doi:10.1073/pnas.77.6.3388. PMC 349621. PMID 6997877.
- Eaton JW, Brandt P, Mahoney JR, Lee JT (February 1982). "Haptoglobin: a natural bacteriostat". Science. 215 (4533): 691–693. Bibcode:1982Sci...215..691E. doi:10.1126/science.7036344. PMID 7036344.
- Kazim AL, Atassi MZ (January 1980). "Haemoglobin binding with haptoglobin. Unequivocal demonstration that the beta-chains of human haemoglobin bind to haptoglobin". The Biochemical Journal. 185 (1): 285–287. doi:10.1042/bj1850285. PMC 1161299. PMID 7378053.
- Hillier LD, Lennon G, Becker M, Bonaldo MF, Chiapelli B, Chissoe S, et al. (September 1996). "Generation and analysis of 280,000 human expressed sequence tags". Genome Research. 6 (9): 807–828. doi:10.1101/gr.6.9.807. PMID 8889549.
- Tabak S, Lev A, Valansi C, Aker O, Shalitin C (November 1996). "Transcriptionally active haptoglobin-related (Hpr) gene in hepatoma G2 and leukemia molt-4 cells". DNA and Cell Biology. 15 (11): 1001–1007. doi:10.1089/dna.1996.15.1001. PMID 8945641.
- Koda Y, Soejima M, Yoshioka N, Kimura H (February 1998). "The haptoglobin-gene deletion responsible for anhaptoglobinemia". American Journal of Human Genetics. 62 (2): 245–252. doi:10.1086/301701. PMC 1376878. PMID 9463309.
External links
edit- Haptoglobins at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P00738 (Haptoglobin) at the PDBe-KB.