Adamantinoma (from Greek adamantinos 'very hard'[1]) is a rare bone cancer, making up less than 1% of all bone cancers.[2] It almost always occurs in the bones of the lower leg[3] and involves both epithelial and osteofibrous tissue.[4]
| Adamantinoma | |
|---|---|
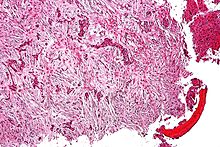 | |
| Micrograph (using H&E stain) of an adamantinoma showing the biphasic histomorphology. | |
| Specialty | Oncology, rheumatology |
Presentation
editPatients typically present with swelling with or without pain. The slow-growing tumor predominantly arises in long bones in a subcortical location (95% in the tibia or fibula).[3]
Benign osteofibrous dysplasia may be a precursor of adamantinoma[4][7] or a regressive phase of adamantinoma.[8]
Histologically, islands of epithelial cells are found in a fibrous stroma. The tumor is typically well-demarcated, osteolytic and eccentric, with cystic zones resembling soap bubbles.[2]
Diagnosis
editX-rays of the affected area show a well defined tumour in bone, with multiple lobules giving a "soap bubble" appearance.[9] MRI can provide a more useful guide to its severity.[9]
Treatment
editTreatment consists of wide resection or amputation. Metastases are rare at presentation but may occur in up to 30% of patients during the disease course. Prognosis is excellent, with overall survival of 85% at 10 years, but is lower when wide surgical margins cannot be obtained. This tumor is insensitive to radiation so chemotherapy is not typically used unless the cancer has metastasized to the lungs or other organs.[2]
History
editThe typically benign odontogenic tumor known as ameloblastoma was first recognized in 1827 by Cusack. Still, it did not yet have any designation. In 1885, this kind of odontogenic neoplasm was designated as an adamantinoma by Malassez.[10] It was finally renamed to the modern name ameloblastoma in 1930 by Ivey and Churchill.[11][12]
References
edit- ^ Brazis PW, Miller NR, Lee AG, Holliday MJ (1995). "Neuro-ophthalmologic Aspects of Ameloblastoma". Skull Base Surg. 5 (4): 233–44. doi:10.1055/s-2008-1058921. PMC 1656531. PMID 17170964.
- ^ a b c Ernest U. Conrad (2008). Orthopaedic Oncology: Diagnosis and Treatment. Thieme. pp. 143–145. ISBN 9781588905239.
- ^ a b Jain D, Jain VK, Vasishta RK, Ranjan P, Kumar Y (2008). "Adamantinoma: A clinicopathological review and update". Diagn Pathol. 3: 8. doi:10.1186/1746-1596-3-8. PMC 2276480. PMID 18279517.
- ^ a b Hatori M, Watanabe M, Hosaka M, Sasano H, Narita M, Kokubun S (May 2006). "A classic adamantinoma arising from osteofibrous dysplasia-like adamantinoma in the lower leg: a case report and review of the literature". Tohoku J. Exp. Med. 209 (1): 53–9. doi:10.1620/tjem.209.53. PMID 16636523.
- ^ "Adamantinoma: Overview - eMedicine". Archived from the original on 25 December 2008. Retrieved 2009-01-04.
- ^ Fischer B. Uber ein primares Adamantinom der Tibia. 12. Frankfurt: Zeitschr. f. Path.; 1913:422-441.
- ^ Springfield DS, Rosenberg AE, Mankin HJ, Mindell ER (1994). "Relationship between osteofibrous dysplasia and adamantinoma". Clin Orthop Relat Res (309): 234–44. PMID 7994967.
- ^ Gleason, Briana C.; Liegl-Atzwanger, Bernadette (2008). "Osteofibrous Dysplasia and Adamantinoma in Children and Adolescents: A Clinicopathologic Reappraisal". American Journal of Surgical Pathology. 32 (3): 363–376. doi:10.1097/PAS.0b013e318150d53e. PMID 18300815. S2CID 22076947.
- ^ a b WHO Classification of Tumours Editorial Board, ed. (2020). "Adamantinoma of long bones". Soft Tissue and Bone Tumours: WHO Classification of Tumours. Vol. 3 (5th ed.). Lyon (France): International Agency for Research on Cancer. pp. 463–466. ISBN 978-92-832-4503-2.
- ^ L. Malassez (1885). "Sur Le role des debris epitheliaux papdentaires". Arch Physiol Norm Pathol. 5: 309–340 6:379–449.
- ^ R.H. Ivey; H.R. Churchill (1930). "The need of a standardized surgical and pathological classification of tumors and anomalies of dental origin". Am Assoc Dent Sch Trans. 7: 240–245.
- ^ Madhup, R; Kirti, S; Bhatt, M; Srivastava, M; Sudhir, S; Srivastava, A (Jan 2006). "Giant ameloblastoma of jaw successfully treated by radiotherapy". Oral Oncology Extra. 42 (1): 22–25. doi:10.1016/j.ooe.2005.08.004.