Nilutamide, sold under the brand names Nilandron and Anandron, is a nonsteroidal antiandrogen (NSAA) which is used in the treatment of prostate cancer.[8][9][10][11][12][13] It has also been studied as a component of feminizing hormone therapy for transgender women and to treat acne and seborrhea in women.[14][15][16][17] It is taken by mouth.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | nye-LOO-tah-mide[1] |
| Trade names | Nilandron, Anandron |
| Other names | RU-23908 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697044 |
| Routes of administration | By mouth[2] |
| Drug class | Nonsteroidal antiandrogen |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Good[2] |
| Protein binding | 80–84%[4] |
| Metabolism | Liver (CYP2C19, FMO)[2][4] |
| Metabolites | At least 5, some active[4][5] |
| Elimination half-life | Mean: 56 hours (~2 days)[6] Range: 23–87 hours[6] |
| Excretion | Urine: 62%[2][4] Feces: <10%[2][4] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.153.268 |
| Chemical and physical data | |
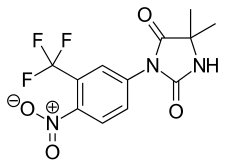
| Formula | C12H10F3N3O4 |
| Molar mass | 317.224 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 149 °C (300 °F) |
| |
| |
| (verify) | |
Side effects in men include breast tenderness and enlargement, feminization, sexual dysfunction, and hot flashes.[18][19][20][21] Nausea, vomiting, visual disturbances, alcohol intolerance, elevated liver enzymes, and lung disease can occur in both sexes.[21][22][19][23][24][25] Rarely, nilutamide can cause respiratory failure and liver damage.[18][21] These unfavorable side effects, along with a number of associated cases of death, have limited the use of nilutamide.[13][26][27]
Nilutamide acts as a selective antagonist of the androgen receptor (AR), preventing the effects of androgens like testosterone and dihydrotestosterone (DHT) in the body.[28][14] Because most prostate cancer cells rely on these hormones for growth and survival, nilutamide can slow the progression of prostate cancer and extend life in men with the disease.[14]
Nilutamide was discovered in 1977 and was first introduced for medical use in 1987.[9][29][30][6] It became available in the United States in 1996.[31][32][33] The drug has largely been replaced by newer and improved NSAAs, namely bicalutamide and enzalutamide, due to their better efficacy, tolerability, and safety, and is now rarely used.[34]
It is on the World Health Organization's List of Essential Medicines.[35]
Medical uses
editProstate cancer
editNilutamide is used in prostate cancer in combination with a gonadotropin-releasing hormone (GnRH) analogue at a dosage of 300 mg/day (150 mg twice daily) for the first 4 weeks of treatment, and 150 mg/day thereafter.[27][36] It is not indicated as a monotherapy in prostate cancer.[27] Only one small non-comparative study has assessed nilutamide as a monotherapy in prostate cancer.[37]
Nilutamide has been used to prevent the effects of the testosterone flare at the start of GnRH agonist therapy in men with prostate cancer.[38][39][40]
Transgender hormone therapy
editNilutamide has been studied for use as a component of feminizing hormone therapy for transgender women.[14][15] It has been assessed in at least five small clinical studies for this purpose in treatment-naive subjects.[15][41][42][43][44][45] In these studies, nilutamide monotherapy at a dosage of 300 mg/day, induced observable signs of clinical feminization in young transgender women (age range 19–33 years) within 8 weeks,[42] including breast development, decreased body hair (though not facial hair),[41] decreased morning erections and sex drive,[43] and positive psychological and emotional changes.[43][46] Signs of breast development occurred in all subjects within 6 weeks and were associated with increased nipple sensitivity,[45][42][43] and along with decreased hair growth, were the earliest sign of feminization.[42]
Nilutamide did not change the size of the prostate gland (which is the same as with high-dosage cyproterone acetate and ethinylestradiol treatment for as long as 18 months), but was found to alter its histology, including increased stromal tissue with a significant reduction in acini and atrophic epithelial cells, indicating glandular atrophy.[44][45][47] In addition, readily apparent histological changes were observed in the testes, including a reduction in tubular and interstitial cells.[44]
Nilutamide was found to more than double luteinizing hormone (LH) and testosterone levels and to triple estradiol levels.[41][42][44] In contrast, follicle-stimulating hormone levels remained unchanged.[42][44] A slight but significant increase in prolactin levels was observed, and levels of sex hormone-binding globulin increased as well.[42][44] The addition of ethinylestradiol to nilutamide therapy after 8 weeks abolished the increase in LH, testosterone, and estradiol levels and dramatically suppressed testosterone levels, into the castrate range.[41][42] Both nilutamide alone and the combination of nilutamide and estrogen were regarded as resulting in effective and favorable antiandrogen action and feminization in transgender women.[41][42]
Skin conditions
editNilutamide has been assessed in the treatment of acne and seborrhea in women in at least one small clinical study.[16][17] The dosage used was 200 mg/day, and in the study, "seborrhea and acne decreased markedly within the first month and practically disappeared after 2 months of [nilutamide] treatment."[16][17]
Available forms
editNilutamide is available in the form of 50 and 150 mg oral tablets.[48]
Side effects
editGeneral side effects of NSAAs, including nilutamide, include gynecomastia, breast pain/tenderness, hot flashes (67%), depression, fatigue, sexual dysfunction (including loss of libido and erectile dysfunction), decreased muscle mass, and decreased bone mass with an associated increase in fractures.[19][20][21] Also, nausea (24–27%), vomiting, constipation (20%), and insomnia (16%) may occur with nilutamide.[21] Nilutamide monotherapy is known to eventually induce gynecomastia in 40 to 80% of men treated with it for prostate cancer, usually within 6 to 9 months of treatment initiation.[49][50][51][52]
Relative to other NSAAs, nilutamide has been uniquely associated with mild and reversible visual disturbances (31–58%) including delayed ocular adaptation to darkness and impaired color vision,[22] a disulfiram-like[19] alcohol intolerance (19%), interstitial pneumonitis (0.77–2.4%)[34][53][54] (which can result in dyspnea (1%) as a secondary effect and can progress to pulmonary fibrosis),[23] and hepatitis (1%), and has a higher incidence of nausea and vomiting compared to other NSAAs.[13][27][21][55] The incidence of interstitial pneumonitis with nilutamide has been found to be much higher in Japanese patients (12.6%), warranting particular caution in Asian individuals.[56][57] There is a case report of simultaneous liver and lung toxicity in a nilutamide-treated patient.[58]
There is also a risk of hepatotoxicity with nilutamide, though occurrence is very rare and the risk is significantly less than with flutamide.[6][59] The incidence of abnormal liver function tests (e.g., elevated liver enzymes) has been variously reported as 2 to 33% with nilutamide.[60][1] For comparison, the risk of elevated liver enzymes has been reported as 4 to 62% in the case of flutamide.[60][24][6] The risk of hepatotoxicity with nilutamide has been described as far less than with flutamide.[1] Fulminant hepatic failure has been reported for nilutamide, with fatal outcome.[6][61][62][63] Between 1986 and 2003, the numbers of published cases of hepatotoxicity for antiandrogens totaled 46 for flutamide, 21 for cyproterone acetate, 4 for nilutamide, and 1 for bicalutamide.[64] Similarly to flutamide, nilutamide exhibits mitochondrial toxicity in hepatocytes by inhibiting respiratory complex I (NADH ubiquinone oxidoreductase) (though not respiratory complexes II, III, or IV) in the electron transport chain, resulting in reduced ATP and glutathione production and thus decreased hepatocyte survival.[63][65][66] The nitro group of nilutamide has been theorized to be involved in both its hepatotoxicity and its pulmonary toxicity.[66][67]
| Class | Side effect | Nilutamide 150 mg/day + orchiectomy (n = 225) (%)a,b |
Placebo + orchi- ectomy (n = 232) (%)a,b |
|---|---|---|---|
| Cardiovascular system | Hypertension | 5.3 | 2.6 |
| Digestive system | Nausea | 9.8 | 6.0 |
| Constipation | 7.1 | 3.9 | |
| Endocrine system | Hot flashes | 28.4 | 22.4 |
| Metabolic and nutritional system | Increased aspartate transaminase | 8.0 | 3.9 |
| Increased alanine transaminase | 7.6 | 4.3 | |
| Nervous system | Dizziness | 7.1 | 3.4 |
| Respiratory system | Dyspnea | 6.2 | 7.3 |
| Special senses | Impaired adaptation to darkness | 12.9 | 1.3 |
| Abnormal vision | 6.7 | 1.7 | |
| Urogenital system | Urinary tract infection | 8.0 | 9.1 |
| Overall | 86 | 81 | |
| Footnotes: a = Phase III studies of combined androgen blockade (nilutamide + orchiectomy) in men with advanced prostate cancer. b = Incidence ≥5% regardless of causality. Sources: See template. | |||
Pharmacology
editPharmacodynamics
editAntiandrogenic activity
edit| Compound | RBA[b] |
|---|---|
| Metribolone | 100 |
| Dihydrotestosterone | 85 |
| Cyproterone acetate | 7.8 |
| Bicalutamide | 1.4 |
| Nilutamide | 0.9 |
| Hydroxyflutamide | 0.57 |
| Flutamide | <0.0057 |
Notes:
| |
Nilutamide acts as a selective competitive silent antagonist of the AR (IC50 = 412 nM),[28] which prevents androgens like testosterone and DHT from activating the receptor.[14] The affinity of nilutamide for the AR is about 1 to 4% of that of testosterone and is similar to that of bicalutamide and 2-hydroxyflutamide.[69][70][71] Similarly to 2-hydroxyflutamide, but unlike bicalutamide, nilutamide is able to weakly activate the AR at high concentrations.[70] It does not inhibit 5α-reductase.[72]
Like other NSAAs such as flutamide and bicalutamide, nilutamide, without concomitant GnRH analogue therapy, increases serum androgen (by two-fold in the case of testosterone), estrogen, and prolactin levels due to inhibition of AR-mediated suppression of steroidogenesis via negative feedback on the hypothalamic–pituitary–gonadal axis.[14] As such, though nilutamide is still effective as an antiandrogen as a monotherapy, it is given in combination with a GnRH analogue such as leuprorelin in prostate cancer to suppress androgen concentrations to castrate levels in order to attain maximal androgen blockade (MAB).[14]
Like flutamide and bicalutamide, nilutamide is able to cross the blood–brain barrier and has central antiandrogen actions.[30]
| Species | IC50 (nM) | RBA (ratio) | ||||
|---|---|---|---|---|---|---|
| Bicalutamide | 2-Hydroxyflutamide | Nilutamide | Bica / 2-OH-flu | Bica / nilu | Ref | |
| Rat | 190 | 700 | ND | 4.0 | ND | [73] |
| Rat | ~400 | ~900 | ~900 | 2.3 | 2.3 | [74] |
| Rat | ND | ND | ND | 3.3 | ND | [75] |
| Rata | 3595 | 4565 | 18620 | 1.3 | 5.2 | [76] |
| Human | ~300 | ~700 | ~500 | 2.5 | 1.6 | [77] |
| Human | ~100 | ~300 | ND | ~3.0 | ND | [78] |
| Humana | 2490 | 2345 | 5300 | 1.0 | 2.1 | [76] |
| Footnotes: a = Controversial data. Sources: See template. | ||||||
Cytochrome P450 inhibition
editNilutamide is known to inhibit several cytochrome P450 enzymes, including CYP1A2, CYP2C9, and CYP3A4, and can result in increased levels of medications that are metabolized by these enzymes.[79] It has also been found to inhibit the enzyme CYP17A1 (17α-hydroxylase/17,20-lyase) in vitro and thus the biosynthesis of androgens.[80][81] However, nilutamide monotherapy significantly increases testosterone levels in vivo, so the clinical significance of this finding is uncertain.[80][81]
Pharmacokinetics
editNilutamide has an elimination half-life of 23 to 87 hours, with a mean of 56 hours,[6] or about two days; this allows for once-daily administration.[13] Steady state (plateau) levels of the drug are attained after two weeks of administration with a dosage of 150 mg twice daily (300 mg/day total).[82] It is metabolized by CYP2C19, with at least five metabolites.[5] Virtually all of the antiandrogenic activity of nilutamide comes from the parent drug (as opposed to metabolites).[83]
Chemistry
editNilutamide is structurally related to the first-generation NSAAs flutamide and bicalutamide as well as to the second-generation NSAAs enzalutamide and apalutamide.
History
editNilutamide was developed by Roussel and was first described in 1977.[9][29][30] It was first introduced for medical use in 1987 in France[6][84] and was the second NSAA to be marketed, with flutamide preceding it and bicalutamide following it in 1995.[13][85] It was not introduced until 1996 in the United States.[31][32][33]
Society and culture
editGeneric names
editNilutamide is the generic name of the drug and its INN, USAN, BAN, and DCF.[9][10][11][12]
Brand names
editNilutamide is marketed under the brand name Nilandron in the United States and under the brand name Anandron elsewhere in the world such as in Australia, Canada, Europe, and Latin America.[10][12]
Availability
editNilutamide is or has been available in the United States, Canada, Australia, Europe, Latin America, Egypt, and Lebanon.[10][12] In Europe, it is or has been available in Belgium, Croatia, the Czech Republic, Finland, France, the Netherlands, Norway, Poland, Portugal, Serbia, Sweden, Switzerland, and Yugoslavia.[10][12] in Latin America, it is or has been available in Argentina, Brazil, and Mexico.[10][12]
Research
editThe combination of an estrogen and nilutamide as a form of combined androgen blockade for the treatment of prostate cancer has been studied in animals.[86]
Nilutamide has been studied in the treatment of advanced breast cancer.[87][88]
References
edit- ^ a b c "Nilutamide - LiverTox". National Institutes of Health. 2012. PMID 31643176. Archived from the original on 24 September 2018. Retrieved 24 September 2018.
In large registration clinical trials, ALT elevations occurred in 2% to 33% of patients during nilutamide therapy. The elevations were usually mild, asymptomatic and transient, rarely requiring drug discontinuation. In rare instances, clinically apparent acute liver injury has occurred during nilutamide therapy, but the number of published cases are few, and the agent appears to be far less hepatotoxic than flutamide.
- ^ a b c d e Perry MC, Doll DC, Freter CE (30 July 2012). Perry's The Chemotherapy Source Book. Lippincott Williams & Wilkins. pp. 711–. ISBN 978-1-4698-0343-2.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ a b c d e f Lemke TL, Williams DA (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1373–. ISBN 978-1-60913-345-0.
- ^ a b Chabner BA, Longo DL (8 November 2010). Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. pp. 680–. ISBN 978-1-60547-431-1. Archived from the original on 10 January 2023. Retrieved 12 October 2016.
- ^ a b c d e f g h Kolvenbag GJ, Furr BJ (2009). "Nonsteroidal Antiandrogens". In Jordan VC, Furr HJ (eds.). Hormone Therapy in Breast and Prostate Cancer. Humana Press. pp. 347–368. doi:10.1007/978-1-59259-152-7_16. ISBN 978-1-60761-471-5.
Although the t1/2 of nilutamide is h (mean 56 h) (39), suggesting that once-daily dosing would be appropriate, a three times per day regimen has been employed in most clinical trials.
- ^ "Nilutamide (Nilandron) Use During Pregnancy". Archived from the original on 28 October 2020. Retrieved 20 July 2016.
- ^ "NILANDRON® (nilutamide)" (PDF). Archived (PDF) from the original on 30 March 2021. Retrieved 25 September 2018.
- ^ a b c d Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 873–. ISBN 978-1-4757-2085-3.
- ^ a b c d e f Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 737–. ISBN 978-3-88763-075-1.
- ^ a b Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 199–. ISBN 978-94-011-4439-1.
- ^ a b c d e f "Nilutamide". Archived from the original on 2 December 2020. Retrieved 14 November 2017.
- ^ a b c d e Denis LJ, Griffiths K, Kaisary AV, Murphy GP (1 March 1999). Textbook of Prostate Cancer: Pathology, Diagnosis and Treatment: Pathology, Diagnosis and Treatment. CRC Press. pp. 280–. ISBN 978-1-85317-422-3. Archived from the original on 10 January 2023. Retrieved 21 February 2016.
- ^ a b c d e f g Denis L (6 December 2012). Antiandrogens in Prostate Cancer: A Key to Tailored Endocrine Treatment. Springer Science & Business Media. pp. 194–210. ISBN 978-3-642-45745-6.
- ^ a b c Kreukels BP, Steensma TD, De Vries AL (1 July 2013). Gender Dysphoria and Disorders of Sex Development: Progress in Care and Knowledge. Springer Science & Business Media. pp. 280–. ISBN 978-1-4614-7441-8.
- ^ a b c Couzinet B, Thomas G, Thalabard JC, Brailly S, Schaison G (July 1989). "Effects of a pure antiandrogen on gonadotropin secretion in normal women and in polycystic ovarian disease". Fertility and Sterility. 52 (1): 42–50. doi:10.1016/s0015-0282(16)60786-0. PMID 2744186.
- ^ a b c Namer M (October 1988). "Clinical applications of antiandrogens". Journal of Steroid Biochemistry. 31 (4B): 719–729. doi:10.1016/0022-4731(88)90023-4. PMID 2462132.
- ^ a b Dole EJ, Holdsworth MT (January 1997). "Nilutamide: an antiandrogen for the treatment of prostate cancer". The Annals of Pharmacotherapy. 31 (1): 65–75. doi:10.1177/106002809703100112. PMID 8997470. S2CID 20347526.
- ^ a b c d Dart RC (2004). Medical Toxicology. Lippincott Williams & Wilkins. pp. 521–. ISBN 978-0-7817-2845-4.
- ^ a b DeAngelis LM, Posner JB (12 September 2008). Neurologic Complications of Cancer. Oxford University Press, USA. pp. 479–. ISBN 978-0-19-971055-3. Archived from the original on 10 January 2023. Retrieved 21 February 2016.
- ^ a b c d e f Lehne RA (2013). Pharmacology for Nursing Care. Elsevier Health Sciences. pp. 1297–. ISBN 978-1-4377-3582-6. Archived from the original on 10 January 2023. Retrieved 12 October 2016.
- ^ a b Becker KL (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1196–. ISBN 978-0-7817-1750-2. Archived from the original on 10 January 2023. Retrieved 12 October 2016.
- ^ a b Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2939–. ISBN 978-1-4160-6911-9. Archived from the original on 10 January 2023. Retrieved 21 February 2016.
- ^ a b Hussain S, Haidar A, Bloom RE, Zayouna N, Piper MH, Jafri SM (2014). "Bicalutamide-induced hepatotoxicity: A rare adverse effect". The American Journal of Case Reports. 15: 266–270. doi:10.12659/AJCR.890679. PMC 4068966. PMID 24967002.
- ^ Boarder MR, Newby D, Navti P (25 March 2010). Pharmacology for Pharmacy and the Health Sciences: A Patient-centred Approach. OUP Oxford. pp. 632–. ISBN 978-0-19-955982-4. Archived from the original on 6 July 2024. Retrieved 12 October 2016.
- ^ DeVita VT, Lawrence TS, Rosenberg SA, eds. (18 March 2016). Prostate and Other Genitourinary Cancers: Cancer: Principles & Practice of Oncology. Wolters Kluwer Health. pp. 1006–. ISBN 978-1-4963-5421-1.
- ^ a b c d Chang C (1 January 2005). Prostate Cancer: Basic Mechanisms and Therapeutic Approaches. World Scientific. pp. 11–. ISBN 978-981-256-920-2.
- ^ a b Singh SM, Gauthier S, Labrie F (February 2000). "Androgen receptor antagonists (antiandrogens): structure-activity relationships". Current Medicinal Chemistry. 7 (2): 211–247. doi:10.2174/0929867003375371. PMID 10637363.
- ^ a b Labrie F, Lagacé L, Ferland L, Kelly PA, Drouin J, Massicotte J, et al. (1978). "Interactions Between LHRH, Sex Steroids and "Inhibin" in the Control of LH and FSH Secretion". International Journal of Andrology. 1 (s2a): 81–101. doi:10.1111/j.1365-2605.1978.tb00008.x. ISSN 0105-6263.
- ^ a b c Raynaud JP, Bonne C, Bouton MM, Lagace L, Labrie F (July 1979). "Action of a non-steroid anti-androgen, RU 23908, in peripheral and central tissues". Journal of Steroid Biochemistry. 11 (1A): 93–99. doi:10.1016/0022-4731(79)90281-4. PMID 385986.
- ^ a b Pavlik EJ (6 December 2012). Estrogens, Progestins, and Their Antagonists: Health Issues. Springer Science & Business Media. pp. 167–. ISBN 978-1-4612-4096-9.
- ^ a b Bohl CE, Gao W, Miller DD, Bell CE, Dalton JT (April 2005). "Structural basis for antagonism and resistance of bicalutamide in prostate cancer". Proceedings of the National Academy of Sciences of the United States of America. 102 (17): 6201–6206. Bibcode:2005PNAS..102.6201B. doi:10.1073/pnas.0500381102. PMC 1087923. PMID 15833816.
- ^ a b "Nilutamide - AdisInsight". Archived from the original on 5 May 2021. Retrieved 26 June 2017.
- ^ a b Gulley JL (2011). Prostate Cancer. Demos Medical Publishing. pp. 81–. ISBN 978-1-935281-91-7.
- ^ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ Upfal J (2006). The Australian Drug Guide: Every Person's Guide to Prescription and Over-the-counter Medicines, Street Drugs, Vaccines, Vitamins and Minerals... Black Inc. pp. 283–. ISBN 978-1-86395-174-6.
- ^ Anderson J (March 2003). "The role of antiandrogen monotherapy in the treatment of prostate cancer". BJU International. 91 (5): 455–461. doi:10.1046/j.1464-410X.2003.04026.x. PMID 12603397. S2CID 8639102.
Trial experience with nilutamide monotherapy is limited to one small non-comparative study involving 26 patients with metastatic disease given nilutamide 100 mg three times daily (the dose used when nilutamide is administered as a component of MAB) [14]. The median progression-free survival in these patients was 9 months, with a median overall survival of 23 months. There have been no comparative trials of nilutamide with other antiandrogens or with castration [15]. The limited available data on nilutamide monotherapy means that no meaningful conclusions about the role of nilutamide in this setting can be determined. Nilutamide is not licensed as monotherapy.
- ^ Thompson IM (2001). "Flare Associated with LHRH-Agonist Therapy". Reviews in Urology. 3 (Suppl 3): S10–S14. PMC 1476081. PMID 16986003.
- ^ Scaletscky R, Smith JA (April 1993). "Disease flare with gonadotrophin-releasing hormone (GnRH) analogues. How serious is it?". Drug Safety. 8 (4): 265–270. doi:10.2165/00002018-199308040-00001. PMID 8481213. S2CID 36964191.
- ^ Kuhn JM, Billebaud T, Navratil H, Moulonguet A, Fiet J, Grise P, et al. (August 1989). "Prevention of the transient adverse effects of a gonadotropin-releasing hormone analogue (buserelin) in metastatic prostatic carcinoma by administration of an antiandrogen (nilutamide)". The New England Journal of Medicine. 321 (7): 413–418. doi:10.1056/NEJM198908173210701. PMID 2503723.
- ^ a b c d e Asscheman H, Gooren LJ, Peereboom-Wynia JD (September 1989). "Reduction in undesired sexual hair growth with anandron in male-to-female transsexuals--experiences with a novel androgen receptor blocker". Clinical and Experimental Dermatology. 14 (5): 361–363. doi:10.1111/j.1365-2230.1989.tb02585.x. PMID 2612040. S2CID 45303518.
- ^ a b c d e f g h i Rao BR, de Voogt HJ, Geldof AA, Gooren LJ, Bouman FG (October 1988). "Merits and considerations in the use of anti-androgen". Journal of Steroid Biochemistry. 31 (4B): 731–737. doi:10.1016/0022-4731(88)90024-6. PMID 3143862.
- ^ a b c d van Kemenade JF, Cohen-Kettenis PT, Cohen L, Gooren LJ (June 1989). "Effects of the pure antiandrogen RU 23.903 (anandron) on sexuality, aggression, and mood in male-to-female transsexuals". Archives of Sexual Behavior. 18 (3): 217–228. doi:10.1007/BF01543196. PMID 2751416. S2CID 44664956.
- ^ a b c d e f Gooren L, Spinder T, Spijkstra JJ, van Kessel H, Smals A, Rao BR, Hoogslag M (April 1987). "Sex steroids and pulsatile luteinizing hormone release in men. Studies in estrogen-treated agonadal subjects and eugonadal subjects treated with a novel nonsteroidal antiandrogen". The Journal of Clinical Endocrinology and Metabolism. 64 (4): 763–770. doi:10.1210/jcem-64-4-763. PMID 3102546.
- ^ a b c de Voogt HJ, Rao BR, Geldof AA, Gooren LJ, Bouman FG (1987). "Androgen action blockade does not result in reduction in size but changes histology of the normal human prostate". The Prostate. 11 (4): 305–311. doi:10.1002/pros.2990110403. PMID 2960959. S2CID 84632739.
- ^ Cohen-Kettenis PT, Gooren LJ (1993). "The Influence of Hormone Treatment on Psychological Functioning of Transsexuals". Journal of Psychology & Human Sexuality. 5 (4): 55–67. doi:10.1300/J056v05n04_04. ISSN 0890-7064. S2CID 145237890.
- ^ Drugs & Aging. Adis International. 1993. Archived from the original on 10 January 2023. Retrieved 2 April 2018.
In 16 male subjects undergoing androgen blockade with nilutamide 100 to 300 mg/day for 8 weeks for male to female gender reassignment, prostate volume was not changed (de Voogt et al. 1987).
- ^ Meyers RA (2 March 2018). Translational Medicine: Molecular Pharmacology and Drug Discovery. Wiley. pp. 46–. ISBN 978-3-527-68719-0. Archived from the original on 10 January 2023. Retrieved 2 August 2018.
- ^ Bautista-Vidal C, Barnoiu O, García-Galisteo E, Gómez-Lechuga P, Baena-González V (2014). "Treatment of gynecomastia in patients with prostate cancer and androgen deprivation". Actas Urologicas Espanolas. 38 (1): 34–40. doi:10.1016/j.acuroe.2013.10.002. PMID 23850393.
[...] the frequency of gynecomastia with antiandrogens in monotherapy is [...] around [...] 79% with nilutamide [...]
- ^ Deepinder F, Braunstein GD (September 2012). "Drug-induced gynecomastia: an evidence-based review". Expert Opinion on Drug Safety. 11 (5): 779–795. doi:10.1517/14740338.2012.712109. PMID 22862307. S2CID 22938364.
Treatment with estrogen has the highest incidence of gynecomastia, at 40 – 80%, anti-androgens, including flutamide, bicalutamide and nilutamide, are next, with a 40 – 70% incidence, followed by GnRH analogs (goserelin, leuprorelin) and combined androgen deprivation [...]
- ^ Michalopoulos NV, Keshtgar MR (October 2012). "Images in clinical medicine. Gynecomastia induced by prostate-cancer treatment". The New England Journal of Medicine. 367 (15): 1449. doi:10.1056/NEJMicm1209166. PMID 23050528.
Gynecomastia occurs in up to 80% of patients who receive nonsteroidal antiandrogens (eg, bicalutamide, flutamide, or nilutamide), usually within the first 6 to 9 months after the initiation of treatment.
- ^ Di Lorenzo G, Autorino R, Perdonà S, De Placido S (December 2005). "Management of gynaecomastia in patients with prostate cancer: a systematic review". The Lancet. Oncology. 6 (12): 972–979. doi:10.1016/S1470-2045(05)70464-2. PMID 16321765.
- ^ Camus P, Rosenow III EC (29 October 2010). Drug-induced and Iatrogenic Respiratory Disease. CRC Press. pp. 235–. ISBN 978-1-4441-2869-7.
- ^ Held-Warmkessel J (2006). Contemporary Issues in Prostate Cancer: A Nursing Perspective. Jones & Bartlett Learning. pp. 257–. ISBN 978-0-7637-3075-8.
- ^ Ramon J, Denis LJ (5 June 2007). Prostate Cancer. Springer Science & Business Media. pp. 229–. ISBN 978-3-540-40901-4.
- ^ Mahler C (1996). "A Review of the Clinical Studies with Nilutamide". Antiandrogens in Prostate Cancer. pp. 105–111. doi:10.1007/978-3-642-45745-6_10. ISBN 978-3-642-45747-0.
Akaza had to prematurely terminate a nilutamide study in Japan as 12.6% of his patients developed interstitial lung disease [4]. This complication has been mainly observed in Japan and much less in other trials worldwide.
- ^ Micromedex (1 January 2003). USP DI 2003: Drug Information for Healthcare Professionals. Thomson Micromedex. pp. 220–224. ISBN 978-1-56363-429-1. Archived from the original on 10 January 2023. Retrieved 12 October 2016.
- ^ Gomez JL, Dupont A, Cusan L, Tremblay M, Tremblay M, Labrie F (May 1992). "Simultaneous liver and lung toxicity related to the nonsteroidal antiandrogen nilutamide (Anandron): a case report". The American Journal of Medicine. 92 (5): 563–566. doi:10.1016/0002-9343(92)90756-2. PMID 1580304.
- ^ Aronson JK (21 February 2009). Meyler's Side Effects of Endocrine and Metabolic Drugs. Elsevier. pp. 150–. ISBN 978-0-08-093292-7.
- ^ a b McLeod DG (1997). "Tolerability of Nonsteroidal Antiandrogens in the Treatment of Advanced Prostate Cancer". The Oncologist. 2 (1): 18–27. doi:10.1634/theoncologist.2-1-18. PMID 10388026.
Incidences of abnormal liver function test results have been variously reported from 2%-33% in nilutamide groups [13, 32, 33, 45] and from 4%-62% in flutamide groups [5, 7, 9, 11, 34, 38-40, 48] in trials of monotherapy and CAB.
- ^ Aronson JK (2011). Side Effects of Drugs Annual: A Worldwide Yearly Survey of New Data in Adverse Drug Reactions. Elsevier. pp. 874–. ISBN 978-0-444-53741-6.
- ^ Marty F, Godart D, Doermann F, Mérillon H (1996). "[Fatal fulminating hepatitis caused by nilutamide. A new case]". Gastroenterologie Clinique et Biologique (in French). 20 (8–9): 710–711. PMID 8977826.
- ^ a b Merwat SN, Kabbani W, Adler DG (April 2009). "Fulminant hepatic failure due to nilutamide hepatotoxicity". Digestive Diseases and Sciences. 54 (4): 910–913. doi:10.1007/s10620-008-0406-8. PMID 18688719. S2CID 27421870.
In addition, nilutamide is noted to exhibit mitochondrial toxicity by inhibiting complex I activity of the mitochondrial respiratory chain leading to the impairment of ATP formation and the biosynthesis of glutathione, thereby possibly predisposing the liver to toxicity [13].
- ^ Chitturi S, Farrell GC (2013). "Adverse Effects of Hormones and Hormone Antagonists on the Liver". Drug-Induced Liver Disease. Vol. 3. Academic Press. pp. 605–619. doi:10.1016/B978-0-12-387817-5.00033-9. ISBN 9780123878175. PMID 11096606.
Liver injury is well recognized with all antiandrogens (Table 33-3). Thus, among all published cases identified between 1986 and 2003, flutamide (46), cyproterone (21), nilutamide (4), and bicalutamide (1) were implicated [107,108].
{{cite book}}:|journal=ignored (help) - ^ Berson A, Schmets L, Fisch C, Fau D, Wolf C, Fromenty B, et al. (July 1994). "Inhibition by nilutamide of the mitochondrial respiratory chain and ATP formation. Possible contribution to the adverse effects of this antiandrogen". The Journal of Pharmacology and Experimental Therapeutics. 270 (1): 167–176. PMID 8035313.
- ^ a b Coe KJ, Jia Y, Ho HK, Rademacher P, Bammler TK, Beyer RP, et al. (September 2007). "Comparison of the cytotoxicity of the nitroaromatic drug flutamide to its cyano analogue in the hepatocyte cell line TAMH: evidence for complex I inhibition and mitochondrial dysfunction using toxicogenomic screening". Chemical Research in Toxicology. 20 (9): 1277–1290. doi:10.1021/tx7001349. PMC 2802183. PMID 17702527.
- ^ Boelsterli UA, Ho HK, Zhou S, Leow KY (October 2006). "Bioactivation and hepatotoxicity of nitroaromatic drugs". Current Drug Metabolism. 7 (7): 715–727. doi:10.2174/138920006778520606. PMID 17073576.
- ^ Ayub M, Levell MJ (August 1989). "The effect of ketoconazole related imidazole drugs and antiandrogens on [3H] R 1881 binding to the prostatic androgen receptor and [3H]5 alpha-dihydrotestosterone and [3H]cortisol binding to plasma proteins". J. Steroid Biochem. 33 (2): 251–5. doi:10.1016/0022-4731(89)90301-4. PMID 2788775.
- ^ Gaillard M (1996). "Pharmacodynamics and Pharmacokinetics of Nilutamide in Animal and Man". Antiandrogens in Prostate Cancer. pp. 95–103. doi:10.1007/978-3-642-45745-6_9. ISBN 978-3-642-45747-0.
- ^ a b Figg W, Chau CH, Small EJ (14 September 2010). Drug Management of Prostate Cancer. Springer Science & Business Media. pp. 71–. ISBN 978-1-60327-829-4. Archived from the original on 10 January 2023. Retrieved 12 October 2016.
- ^ Benni HJ, Vemer HM (15 December 1990). Chronic Hyperandrogenic Anovulation. CRC Press. pp. 153–. ISBN 978-1-85070-322-8.
- ^ Raynaud JP, Fiet J, Le Goff JM, Martin PM, Moguilewsky M, Ojasoo T (1987). "Design of antiandrogens and their mechanisms of action: a case study (anandron)". Hormone Research. 28 (2–4): 230–241. doi:10.1159/000180948 (inactive 11 November 2024). PMID 3331376.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H (June 1987). "ICI 176,334: a novel non-steroidal, peripherally selective antiandrogen". The Journal of Endocrinology. 113 (3): R7–R9. doi:10.1677/joe.0.113R007. PMID 3625091.
- ^ Teutsch G, Goubet F, Battmann T, Bonfils A, Bouchoux F, Cerede E, Gofflo D, Gaillard-Kelly M, Philibert D (January 1994). "Non-steroidal antiandrogens: synthesis and biological profile of high-affinity ligands for the androgen receptor". The Journal of Steroid Biochemistry and Molecular Biology. 48 (1): 111–119. doi:10.1016/0960-0760(94)90257-7. PMID 8136296. S2CID 31404295.
- ^ Winneker RC, Wagner MM, Batzold FH (December 1989). "Studies on the mechanism of action of Win 49596: a steroidal androgen receptor antagonist". Journal of Steroid Biochemistry. 33 (6): 1133–1138. doi:10.1016/0022-4731(89)90420-2. PMID 2615358.
- ^ a b Luo S, Martel C, Leblanc G, Candas B, Singh SM, Labrie C, Simard J, Bélanger A, Labrie F (1996). "Relative potencies of Flutamide and Casodex: preclinical studies". Endocrine Related Cancer. 3 (3): 229–241. doi:10.1677/erc.0.0030229. ISSN 1351-0088.
- ^ Ayub M, Levell MJ (August 1989). "The effect of ketoconazole related imidazole drugs and antiandrogens on [3H] R 1881 binding to the prostatic androgen receptor and [3H]5 alpha-dihydrotestosterone and [3H]cortisol binding to plasma proteins". Journal of Steroid Biochemistry. 33 (2): 251–255. doi:10.1016/0022-4731(89)90301-4. PMID 2788775.
- ^ Kemppainen JA, Wilson EM (July 1996). "Agonist and antagonist activities of hydroxyflutamide and Casodex relate to androgen receptor stabilization". Urology. 48 (1): 157–163. doi:10.1016/S0090-4295(96)00117-3. PMID 8693644.
- ^ Ferrando SJ, Levenson JL, Owen JA (20 May 2010). Clinical Manual of Psychopharmacology in the Medically Ill. American Psychiatric Pub. pp. 256–. ISBN 978-1-58562-942-8.
- ^ a b Harris MG, Coleman SG, Faulds D, Chrisp P (1993). "Nilutamide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in prostate cancer". Drugs & Aging. 3 (1): 9–25. doi:10.2165/00002512-199303010-00002. PMID 8453188. S2CID 262029302.
- ^ a b Ayub M, Levell MJ (July 1987). "Inhibition of rat testicular 17 alpha-hydroxylase and 17,20-lyase activities by anti-androgens (flutamide, hydroxyflutamide, RU23908, cyproterone acetate) in vitro". Journal of Steroid Biochemistry. 28 (1): 43–47. doi:10.1016/0022-4731(87)90122-1. PMID 2956461.
- ^ Denis L (6 December 2012). Antiandrogens in Prostate Cancer: A Key to Tailored Endocrine Treatment. Springer Science & Business Media. pp. 202–. ISBN 978-3-642-45745-6.
The plateau level of nilutamide (steady state) was obtained after about 14 days of repeated administration of the drug (150 mg b.i.d.) and did not depend upon intervals between doses.
- ^ Mahler C, Verhelst J, Denis L (May 1998). "Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer". Clinical Pharmacokinetics. 34 (5): 405–417. doi:10.2165/00003088-199834050-00005. PMID 9592622. S2CID 25200595.
- ^ Fischer J, Klein C, Childers WE (16 April 2018). Successful Drug Discovery. Wiley. pp. 98–. ISBN 978-3-527-80868-7.
- ^ Wellington K, Keam SJ (2006). "Bicalutamide 150mg: a review of its use in the treatment of locally advanced prostate cancer". Drugs. 66 (6): 837–850. doi:10.2165/00003495-200666060-00007. PMID 16706554. S2CID 46966712.
- ^ Rao BR, Geldof AA, van der Wilt CL, de Voogt HJ (1988). "Efficacy and advantages in the use of low doses of Anandron and estrogen combination in the treatment of prostate cancer". The Prostate. 13 (1): 69–78. doi:10.1002/pros.2990130108. PMID 3420036. S2CID 23553575.
- ^ Chia K, O'Brien M, Brown M, Lim E (February 2015). "Targeting the androgen receptor in breast cancer". Current Oncology Reports. 17 (2): 4. doi:10.1007/s11912-014-0427-8. PMID 25665553. S2CID 5174768.
- ^ Millward MJ, Cantwell BM, Dowsett M, Carmichael J, Harris AL (May 1991). "Phase II clinical and endocrine study of Anandron (RU-23908) in advanced post-menopausal breast cancer". British Journal of Cancer. 63 (5): 763–764. doi:10.1038/bjc.1991.170. PMC 1972372. PMID 1903951.
Further reading
edit- Raynaud JP, Bonne C, Moguilewsky M, Lefebvre FA, Bélanger A, Labrie F (1984). "The pure antiandrogen RU 23908 (Anandron), a candidate of choice for the combined antihormonal treatment of prostatic cancer: a review". The Prostate. 5 (3): 299–311. doi:10.1002/pros.2990050307. PMID 6374639. S2CID 85417869.
- Moguilewsky M, Bertagna C, Hucher M (1987). "Pharmacological and clinical studies of the antiandrogen Anandron". Journal of Steroid Biochemistry. 27 (4–6): 871–875. doi:10.1016/0022-4731(87)90162-2. PMID 3320565.
- Du Plessis DJ (1991). "Castration plus nilutamide vs castration plus placebo in advanced prostate cancer. A review". Urology. 37 (2 Suppl): 20–24. doi:10.1016/0090-4295(91)80097-q. PMID 1992599.
- Creaven PJ, Pendyala L, Tremblay D (1991). "Pharmacokinetics and metabolism of nilutamide". Urology. 37 (2 Suppl): 13–19. doi:10.1016/0090-4295(91)80096-p. PMID 1992598.
- Harris MG, Coleman SG, Faulds D, Chrisp P (1993). "Nilutamide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in prostate cancer". Drugs & Aging. 3 (1): 9–25. doi:10.2165/00002512-199303010-00002. PMID 8453188. S2CID 262029302.
- Dole EJ, Holdsworth MT (January 1997). "Nilutamide: an antiandrogen for the treatment of prostate cancer". The Annals of Pharmacotherapy. 31 (1): 65–75. doi:10.1177/106002809703100112. PMID 8997470. S2CID 20347526.
- Iversen P, Melezinek I, Schmidt A (January 2001). "Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function". BJU International. 87 (1): 47–56. doi:10.1046/j.1464-410x.2001.00988.x. PMID 11121992. S2CID 28215804.