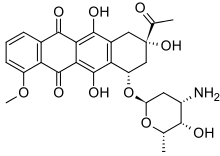
Daunorubicin, also known as daunomycin, is a chemotherapy medication used to treat cancer.[2] Specifically it is used for acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myelogenous leukemia (CML), and Kaposi's sarcoma.[2] It is administered by injection into a vein.[2] A liposomal formulation known as liposomal daunorubicin also exists.[2]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Cerubidine, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682289 |
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Liver |
| Elimination half-life | 26.7 hours (metabolite) |
| Excretion | Bile duct and urinary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.040.048 |
| Chemical and physical data | |
| Formula | C27H29NO10 |
| Molar mass | 527.526 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Common side effects include hair loss, vomiting, bone marrow suppression, and inflammation of the inside of the mouth.[2] Other severe side effects include heart disease and tissue death at the site of injection.[2] Use in pregnancy may harm the fetus.[2] Daunorubicin is in the anthracycline family of medication.[3] It works in part by blocking the function of topoisomerase II.[2]
Daunorubicin was approved for medical use in the United States in 1979.[2] It is on the World Health Organization's List of Essential Medicines.[4] It was originally isolated from bacteria of the Streptomyces type.[5]
Medical uses
editIt slows or stops the growth of cancer cells in the body. Treatment is usually performed together with other chemotherapy drugs (such as cytarabine), and its administration depends on the type of tumor and the degree of response.[citation needed]
In addition to its major use in treating acute myeloid leukemia, daunorubicin is also used to treat neuroblastoma. Daunorubicin has been used with other chemotherapy agents to treat the blastic phase of chronic myelogenous leukemia.[citation needed]
Daunorubicin is also used as the starting material for semi-synthetic manufacturing of doxorubicin, epirubicin and idarubicin.[citation needed]
Mechanism of action
editSimilar to doxorubicin, daunorubicin interacts with DNA by intercalation and inhibition of macromolecular biosynthesis.[6][7] This inhibits the progression of the enzyme topoisomerase II, which relaxes supercoils in DNA; without action of topoisomerase II, these DNA supercoils interfere in transcription of DNA. Daunorubicin stabilizes the topoisomerase II complex after it has broken the DNA chain for replication, preventing the DNA double helix from being resealed and thereby stopping the process of replication. On binding to DNA, daunomycin intercalates, with its daunosamine residue directed toward the minor groove. It has the highest preference for two adjacent G/C base pairs flanked on the 5' side by an A/T base pair. Crystallography shows that daunomycin induces a local unwinding angle of 8°, and other conformational disturbances of adjacent and second-neighbour base pairs.[8] It can also induce histone eviction from chromatin upon intercalation.[9][10]
History
editIn the 1950s, an Italian research company, Farmitalia Research Laboratories, began an organized effort to isolate anticancer compounds from soil-based microbes. A soil sample was isolated from the area surrounding the Castel del Monte, a 13th-century castle in Apulia. A new strain of Streptomyces peucetius which produced a red pigment was isolated, and an antibiotic was produced from this bacterium that was found to have good activity against murine tumors. Since a group of French researchers discovered the same compound at about the same time, the two teams named the compound daunorubicin, combining the name Dauni, a pre-Roman tribe that occupied the area of Italy where the compound was isolated, with the French word for ruby, rubis, describing the color.[11][12][13] Clinical trials began in the 1960s, and the drug saw success in treating acute leukemia and lymphoma.
However, by 1967, it was recognized that daunorubicin could produce fatal cardiac toxicity.[14]
In 2015–16, a team at Ohio State University "showed that, by carefully manipulating strands of viral DNA, an origami structure with complex folds can be created in just 10 minutes. Incredibly, these structures are only 100 nanometers across – that’s 1,000 times smaller than the width of a human hair. Small volumes of daunorubicin can be wrapped up in these minuscule pods, which can then be released into a leukemia cell-filled environment."[15][16][unreliable medical source?]
Route of administration
editDaunorubicin should only be administered in a rapid intravenous infusion. It should not be administered intramuscularly or subcutaneously, since it may cause extensive tissue necrosis. It should also never be administered intrathecally (into the spinal canal), as this will cause extensive damage to the nervous system and may lead to death. Daunorubicin has been used intravitreally (inside the eye) for the purposes of preventing proliferative vitreoretinopathy, a common complication following retinal detachment surgery, but has not been found to be effective and is not used for any other ophthalmic purposes at this time.[17]
References
edit- ^ "Daunorubicin (Cerubidine) Use During Pregnancy". Drugs.com. 19 September 2019. Retrieved 15 August 2020.
- ^ a b c d e f g h i "Daunorubicin hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 8 January 2017. Retrieved 8 December 2016.
- ^ British National Formulary: BNF 69 (69th ed.). British Medical Association. 2015. pp. 581–583. ISBN 9780857111562.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Lin GQ, You QD, Cheng JF (2011). Chiral Drugs: Chemistry and Biological Action. John Wiley & Sons. p. 120. ISBN 9781118075630. Archived from the original on 21 December 2016.
- ^ Fornari FA, Randolph JK, Yalowich JC, Ritke MK, Gewirtz DA (April 1994). "Interference by doxorubicin with DNA unwinding in MCF-7 breast tumor cells". Molecular Pharmacology. 45 (4): 649–656. PMID 8183243.
- ^ Momparler RL, Karon M, Siegel SE, Avila F (August 1976). "Effect of adriamycin on DNA, RNA, and protein synthesis in cell-free systems and intact cells". Cancer Research. 36 (8): 2891–2895. PMID 1277199. Archived from the original on 5 February 2009.
- ^ Quigley GJ, Wang AH, Ughetto G, van der Marel G, van Boom JH, Rich A (December 1980). "Molecular structure of an anticancer drug-DNA complex: daunomycin plus d(CpGpTpApCpG)". Proceedings of the National Academy of Sciences of the United States of America. 77 (12): 7204–7208. Bibcode:1980PNAS...77.7204Q. doi:10.1073/pnas.77.12.7204. PMC 350470. PMID 6938965.
- ^ Pang B, Qiao X, Janssen L, Velds A, Groothuis T, Kerkhoven R, et al. (2013). "Drug-induced histone eviction from open chromatin contributes to the chemotherapeutic effects of doxorubicin". Nature Communications. 4: 1908. Bibcode:2013NatCo...4.1908P. doi:10.1038/ncomms2921. PMC 3674280. PMID 23715267.
- ^ Pang B, de Jong J, Qiao X, Wessels LF, Neefjes J (July 2015). "Chemical profiling of the genome with anti-cancer drugs defines target specificities". Nature Chemical Biology. 11 (7): 472–480. doi:10.1038/nchembio.1811. PMID 25961671.
- ^ Weiss RB (December 1992). "The anthracyclines: will we ever find a better doxorubicin?". Seminars in Oncology. 19 (6): 670–686. PMID 1462166.
- ^ Baruffa G (1966). "Clinical trials in Plasmodium falciparum malaria with a long-acting sulphonamide". Transactions of the Royal Society of Tropical Medicine and Hygiene. 60 (2): 222–224. doi:10.1016/0035-9203(66)90030-7. PMID 5332105.
- ^ Camerino B, Palamidessi G (1960). "Derivati della parazina II. Sulfonamdopir" [Derivatives of parazine II. Sulfonamdopir]. Gazzetta Chimica Italiana [Italian Chemical Journal] (in Italian). 90: 1802–1815.
- ^ Tan C, Tasaka H, Yu KP, Murphy ML, Karnofsky DA (March 1967). "Daunomycin, an antitumor antibiotic, in the treatment of neoplastic disease. Clinical evaluation with special reference to childhood leukemia". Cancer. 20 (3): 333–353. doi:10.1002/1097-0142(1967)20:3<333::AID-CNCR2820200302>3.0.CO;2-K. PMID 4290058. S2CID 19272219.
- ^ "Researchers kill drug-resistant leukemia cells using DNA Trojan horse attack". IFL Science. 25 February 2016.
- ^ Halley PD, Lucas CR, McWilliams EM, Webber MJ, Patton RA, Kural C, et al. (January 2016). "Daunorubicin-Loaded DNA Origami Nanostructures Circumvent Drug-Resistance Mechanisms in a Leukemia Model". Small. 12 (3): 308–320. doi:10.1002/smll.201502118. PMC 4879968. PMID 26583570.
- ^ Mortensen ME, Cecalupo AJ, Lo WD, Egorin MJ, Batley R (1992). "Inadvertent intrathecal injection of daunorubicin with fatal outcome". Medical and Pediatric Oncology. 20 (3): 249–253. doi:10.1002/mpo.2950200315. PMID 1574039.