Thrombosis prevention or thromboprophylaxis is medical treatment to prevent the development of thrombosis (blood clots inside blood vessels) in those considered at risk for developing thrombosis.[1] Some people are at a higher risk for the formation of blood clots than others, such as those with cancer undergoing a surgical procedure.[2][3] Prevention measures or interventions are usually begun after surgery as the associated immobility will increase a person's risk.[4]
| Thrombosis prevention | |
|---|---|
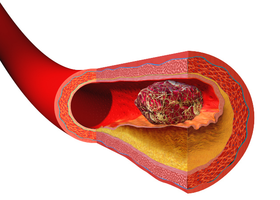 A blood clot blocking a blood vessel. | |
| Other names | Thrombosis prophylaxis |
| ICD-10-PCS | I80-I82 |
| ICD-9-CM | 437.6, 453, 671.5, 671.9 |
Blood thinners are used to prevent clots, these blood thinners have different effectiveness and safety profiles. A 2018 systematic review found 20 studies that included 9771 people with cancer. The evidence did not identify any difference between the effects of different blood thinners on death, developing a clot, or bleeding.[2] A 2021 review found that low molecular weight heparin (LMWH) was superior to unfractionated heparin in the initial treatment of venous thromboembolism for people with cancer.[3]
There are medication-based interventions and non-medication-based interventions.[4] The risk of developing blood clots can be lowered by life style modifications, the discontinuation of oral contraceptives, and weight loss. In those at high risk both interventions are often used.[1] The treatments to prevent the formation of blood clots is balanced against the risk of bleeding.[5]
One of the goals of blood clot prevention is to limit venous stasis as this is a significant risk factor for forming blood clots in the deep veins of the legs.[6] Venous stasis can occur during the long periods of not moving. Thrombosis prevention is also recommended during air travel.[7] Thrombosis prophylaxis is effective in preventing the formation of blood clots, their lodging in the veins, and their developing into thromboemboli that can travel through the circulatory system to cause blockage and subsequent tissue death in other organs.[1] Clarence Crafoord is credited with the first use of thrombosis prophylaxis in the 1930s.
Pathophysiology of blood clot prevention
editThe development of blood clots can be interrupted and prevented by the use of medication, changing risk factors and other interventions. Some risk factors can be modified. These would be losing weight, increasing exercise and the cessation of oral contraceptives. Moving during periods of travel is a modifiable behavior. Preventing blood clots includes the use of medications that interrupt the complex clotting cascade and changing the proteins that are needed for clotting. Antiplatelet drugs also have an effect in preventing the formation of clots.[citation needed]
Medical treatments
editThrombosis prophylaxis is not only used for the prevention of deep vein thrombosis, but can be initiated for the prevention of the formation of blood clots in other organs and circumstances unrelated to deep vein thrombosis:[citation needed]
- cerebral complications
- abortion
- ectopic pregnancy
- molar pregnancy
- pregnancy
- childbirth and the puerperium
- coronary
- portal vein thrombosis
- intracranial, nonpyogenic
- intraspinal, nonpyogenic
- mesenteric
- pulmonary[8][9]
Epidemiology of developing blood clots
editThe risk of developing deep vein thrombosis, or pulmonary embolism is different than the total risk of the formation of blood clots. This is due to the observation that not all blood clots form in the lower legs. Most hospitalized medical patients have at least 1 risk factor for thrombosis that progresses to thromboembolism and this risk persists weeks after discharge. Those who remain undiagnosed and not treated prophylactically have a 26% chance of developing a fatal embolism. Another 26% develop another embolism. Between 5% and 10% of all in hospital deaths are due to pulmonary embolism (as a consequence of thrombosis). Estimates of the incidence of pulmonary embolism in the US is 0.1% persons/year. Hospital admissions in the US for pulmonary embolism are 200,000 to 300,000 yearly.[10] Thrombosis that develops into DVT will affect 900,000 people and kill up to 100,000 in the US. On average 28,726 hospitalized adults aged 18 and older with a VTE blood clot diagnosis die each year.[11] Risk of thrombosis is related to hospitalization.[4] In 2005 the UK the Parliamentary Health Select Committee determined the annual rate of death due to thrombosis was 25,000 with at least 50% being hospital-acquired.[12]
The type of surgery performed prior to the formation of blood clots influences the risk. Without prophylactic interventions, the calculated incidence of clot formation in the lower leg veins after surgery is:
- 22% for neurosurgery
- 26% for abdominal surgery
- 45% for 60% in orthopedic surgery
- 14% for gynecologic surgery[13]
As the population of the US ages, the development of blood clots is becoming more common.[14]
General risks and indications for blood clot prevention
editSome risk factors for developing blood clots are considered higher that others. One scoring system analyzes the probability for clot formation by assigning a point value system to significant risk factors.[15] The benefit of treating those who are at low risk of developing blood clots may not outweigh the higher risks of significant bleeding.[16]
Risk factors for developing blood clots that are assessed prior to treatments
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Probability and risk estimation for developing blood clots Major risk (=1 point) Minor risk (=2 points) Cancer Family history of
deep vein thrombosisImmobility Hospitalization within
the past 6 monthsCalf swelling superficial vein dilation Recent major surgery redness of area Edema or swelling of only leg Recent trauma
to legTenderness in
the calf and/or thigh
| Probability determination and scoring |
|---|
| High probability scoring (12–7 points |
| 3 major points OR 2 major points AND >2 minor points |
| Low probability scoring (3–5 points) |
| 0 major points AND > 2 minor points 1 major point AND >2 minor points 0 major points and >3 minor point 1 major point and more than one minor point |
| Moderate probability scoring (varies) |
| all other risk combinations |
Risk for subsequent blood clots
editDeveloping blood clots is more probable after the first episode. Risk assessment and intervention for those with one or more episodes of deep vein thrombosis or blood clots in the veins utilizes the Well's test. It has been inconsistently modified by a number of publishers with the results listed below:[28]
Well's and modified Well's risk scoring
edit| Finding | points | references |
|---|---|---|
| D-dimer abonormal one month after stopping anticoagulants | 2 | [28] |
| Age > or = to 50 | 1 | [28] |
| male | 1 | [28] |
| use of hormone at DVT onset | 1 | [28] |
Adapted for the emergency department
edit| Finding | points | references |
|---|---|---|
| Malignancy | 1 | [29] |
| Age > or = to 50 | 1 | [29] |
| cast on lower leg/Paralysis/paresis/ | 1 | [29] |
| Recent surgery or immobility | 1 | [29] |
| tenderness over deep vein | 1 | [29] |
| entire leg swollen | 1 | [29] |
| difference of 3 cm between legs | 1 | [29] |
| pitting edema of affected leg | 1 | [29] |
| Collateral superficial veins | 1 | [29] |
| another diagnosis more probable than DVT | −2 | [29] |
Scoring:
- less than 2 points – low risk (3%)
- 2–6 points moderate risk (17%)
- > 6 points high risk (75%)[29]
General interventions
editThe Centers for Disease Control and Prevention have issued general guidelines describing the interventions that can be taken to reduce the risk of the formation of blood clots:
The Centers for Disease Control and Prevention recommend the following:
- Move around as soon as possible after having been confined to bed, such as after surgery, illness, or injury.
- If you're at risk for DVT, talk to your doctor about:
- Graduated compression stockings (sometimes called "medical compression stockings")
- Medication (anticoagulants) to prevent DVT.
- When sitting for long periods of time, such as when traveling for more than four hours:
- Get up and walk around every 2 to 3 hours.
- Exercise your legs while you're sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Raising and lowering your toes while keeping your heels on the floor
- Tightening and releasing your leg muscles
- Wear loose-fitting clothes.
- You can reduce your risk by maintaining a healthy weight, avoiding a sedentary lifestyle, and following your doctor's recommendations based on your individual risk factors.[7]
Interventions during travel
editSeat-edge pressure from the seat on an airplane on the popliteal area may contribute to vessel wall damage as well as venous stasis. Coagulation activation may result from an interaction between cabin conditions (such as hypobaric hypoxia) and individual risk factors for the formation of blood clots. Studies of the pathophysiologic mechanisms for the increased risk of Venous thrombosis embolism or VTE after long-distance travel have not produced consistent results, but venous stasis appears to play a major role; other factors specific to air travel may increase coagulation activation, particularly in passengers with individual risk factors for VTE.[30]
Interventions for those hospitalized
editCompression devices
editMechanical compression devices are used for prevention of thrombosis and are beneficial enough to be used by themselves with patients at low to moderate risk.[4] The use of fitted intermittent pneumatic compression devices before, during and after procedures is used in inpatient settings. It consists of an air pump and inflatable auxiliary compartments that sequentially inflates and deflated to provide an external 'pump' that returns venous blood toward the heart.[31] The use of intermittent pneumatic compression is common.[31][19][5] These devices are also placed on a surgical patient in the operating room (the intra-surgical period) and remain on the person while recovering from the surgery.[32]
The application of antiembolism stockings can be used to prevent thrombosis.[4] The correct use and properly fitted graded compression stockings can reduce the rate of thrombosis by 50%.[15][19]: 745–46 Contraindications for the use of antiembolism stockings include the presence of advanced peripheral and obstructive arterial disease, septic phlebitis, heart failure, open wounds, dermatitis and peripheral neuropathy.[33] Differences between the use of thigh-high compression stockings and shorter types to prevent blood clots exist, but remain inconsistent.[4][5]
Assessment
editThere has been some success in preventing blood clots by an early risk assessment upon admission to the hospital, which is a strategy recognized by the Centers for Disease Control and Prevention. Hospitals that have participated in this effort to reduce the incidence of thrombosis found that rates of DVT decreased in some instances.[34] Some hospitals developed a mandatory assessment quantifying the risk for developing blood clots and a plan of care developed from the results. The person's risk for developing blood clots is entered into their record, 'following' them through their treatment regime. If the hospital stay exceeds three days, the person will be reassessed for risk. Clinicians are then able to apply protocols for prevention based upon best clinical practices.[35][36]
Interventions to treat immobility
editImmobility is a significant risk factor in the development of thrombosis.[37][38][22][25] Immediate post-surgical interventions, such as out of bed orders (OOB), are typically ordered by the physician to prevent thrombosis. These orders, typically delegated to a nurse, but may include the participation of a physical therapist and others trained to perform the intervention, are to perform range of motion (ROM) activities that include: muscle contractions of the lower legs for those who are very weak, moving the feet, wiggling the toes, bending the knees, raise and lower the legs. In addition, changes in positioning prevents immobility and shifts areas of venous stasis. If the person is too weak to perform these preventative activities, hospital personnel will perform these movements independently. Exercise of the lower extremities is a post-operative method of prophylaxis. Nursing personnel will often perform range of motion exercises and encourage frequent moving of the legs, feet, and ankles. Frequent positioning changes and adequate fluid intake. After a surgical procedure, ambulation as soon as possible is prophylactic in preventing the formation of blood clots.[38][22][25]
Early ambulation also prevents venous stasis and physicians order OOB activities on the same day of surgery. This is accomplished in increments. The progression of increasing mobility proceeds by: raising the head of the bed, sitting up in bed, moving to the edge of the bed, dangling the legs off the bed and then ambulating to a close chair.[19][25]
Patient education and compliance reduces the risk of developing blood clots. These exercises and use of equipment and follow up by clinicians reduces the risk of developing blood clots.[25]
Note that if a blood clot has already formed in the deep veins of the leg, bedrest is usually prescribed and the treatment to prevent bloods with physical intervention is contraindicated.[citation needed]
Medication
editAnticoagulants and antiplatelets
editThromboprophylaxis, such as anticoagulants or perioperative heparin, is effective for hospitalized patients at risk for VTE.[2][39] Additional risk factors such as obesity, disease, malignancies, long surgeries, and immobility may influence the prescribed dosage. Anticoagulant medications may prevent the formation of blood clots in people who are at high risk for their development.[4] Treating blood clots that have already formed is managed by the use of anti-hemolytic ("clot busters"). Despite its effectiveness, the use of thromboprophylaxis remains under-utilized, though alerts (computer or human) in hospitals are associated with increased prescription and reductions in symptomatic VTE.[39] The list below describes some of the more common medications used to prevent blood clots.[24] Note that generally since blood clotting is inhibited, a side effect typically is increased bleeding, though it can be reversed by administering a medication that stops the bleeding or by discontinuation of the medication itself. Anti-coagulant administration is often given before the start of the operation.[25] Medications that inhibit blood clot formation include:
Medications used to prevent blood clots
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Heparins
editAdding heparin to the use of compression stockings may prevent thrombosis for those of higher risk.[4][47]
This section may require cleanup to meet Wikipedia's quality standards. The specific problem is: Unclear colors and separation. (December 2022) |
The discontinuation of contraceptives also prevents blood clots.[15]
Herbal interactions
editThe therapeutic effects of warfarin may be decreased by valerian. Anticoagulants can be affected by chamomile. Dong quai, garlic, ginger, Ginkgo biloba, bilberry and feverfew can increase bleeding time. These same herbal supplements taken with warfarin increased prothrombin time.[24]
Dietary interactions
editBy containing significant content of vitamin K, some foods act as antagonists to antiplatelet and anticoagulant medications; these include green leafy vegetables, like spinach, legumes, and broccoli.[24]
Contraindications
editPreventing blood clots with medication is not considered safe in the following circumstances:
- uncooperative patient
- recent childbirth
- gastrointestinal bleeding
- reproductive system
bleeding - genitourinary system
bleeding - hemorrhagic blood dyscrasias
- peptic ulcers
- alcoholism
- infection
- eye surgery
- brain surgery
- spinal cord surgery
- recent cerebrovascular hemorrhage[1]: 877
Research
editAn international registry and risk assessment calculator is being used to centralize data on post-surgical venous thrombosis and its prevention.[53] Hospitals are implementing a multi-disciplinary approach to prevent of blood clots. This includes adequate assessment of the risks, follow up on missed doses of medication and instituting a 'patient-centered' approach endorsed by the Joint Commission.[34] Recommendations regarding the prevention of blood clots vary widely between clinicians and treatment facilities. Research continues to clarify these discrepancies.[5] The metabolic state of hypercoagulability (the tendency to form blood clots) tests are being developed. These include the evaluation of the thrombin–antithrombin complexes (TAT), low levels of the anticoagulants ATIII and protein C, but these tests are not yet widely available.[13]
References
edit- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab Brunner L (2010). Brunner & Suddarth's textbook of medical-surgical nursing. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 876. ISBN 978-0781785907.
- ^ a b c d Matar CF, Kahale LA, Hakoum MB, Tsolakian IG, Etxeandia-Ikobaltzeta I, Yosuico VE, et al. (July 2018). "Anticoagulation for perioperative thromboprophylaxis in people with cancer". The Cochrane Database of Systematic Reviews. 2019 (7): CD009447. doi:10.1002/14651858.cd009447.pub3. PMC 6389341. PMID 29993117.
- ^ a b Kahale, Lara A.; Matar, Charbel F.; Hakoum, Maram B.; Tsolakian, Ibrahim G.; Yosuico, Victor Ed; Terrenato, Irene; Sperati, Francesca; Barba, Maddalena; Schünemann, Holger; Akl, Elie A. (December 8, 2021). "Anticoagulation for the initial treatment of venous thromboembolism in people with cancer". The Cochrane Database of Systematic Reviews. 2021 (12): CD006649. doi:10.1002/14651858.CD006649.pub8. ISSN 1469-493X. PMC 8653422. PMID 34878173.
- ^ a b c d e f g h i Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, Baigent C (December 2005). "Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis". Health Technology Assessment. 9 (49): iii–iv, ix–x, 1–78. doi:10.3310/hta9490. PMID 16336844.
- ^ a b c d Grotta J (2016). Stroke : pathophysiology, diagnosis, and management. Philadelphia: Elsevier. pp. 953–62. ISBN 978-0323295444.
- ^ Martinelli I, Bucciarelli P, Mannucci PM (February 2010). "Thrombotic risk factors: basic pathophysiology". Critical Care Medicine. 38 (2 Suppl): S3-9. doi:10.1097/CCM.0b013e3181c9cbd9. PMID 20083911. S2CID 34486553.
- ^ a b "Venous Thromboembolism (Blood Clots) Facts". Division of Blood Disorders National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. February 24, 2016. Retrieved July 19, 2016. This article incorporates text from this source, which is in the public domain.
- ^ "ICD-10 Version:2016". International Statistical Classification of Diseases and Related Health Problems 10th Revision. Retrieved December 18, 2016.
- ^ Leveno K (2013). Williams manual of pregnancy complications. New York: McGraw-Hill Medical. ISBN 978-0071765626.
- ^ Kafeza M, Shalhoub J, Salooja N, Bingham L, Spagou K, Davies AH (September 2017). "A systematic review of clinical prediction scores for deep vein thrombosis". Phlebology. 32 (8): 516–531. doi:10.1177/0268355516678729. hdl:10044/1/41102. PMID 27885107. S2CID 13759574.
- ^ "Venous Thromboembolism (VTE)" (PDF). National Center on Birth Defects and Developmental Disabilities. Archived from the original (PDF) on October 23, 2018. This article incorporates text from this source, which is in the public domain.
- ^ Hunt BJ (March 2008). "Awareness and politics of venous thromboembolism in the United kingdom". Arteriosclerosis, Thrombosis, and Vascular Biology. 28 (3): 398–9. doi:10.1161/ATVBAHA.108.162586. PMID 18296598.
- ^ a b c d Newman M (2008). Perioperative medicine : managing for outcome. Philadelphia: Saunders Elsevier. pp. 29–34. ISBN 978-1437721263.
- ^ a b c d e f g h i j k l m n Henke PK, Meissner MH, Wakefield TW. "Chapter 2: Risk Factors for Venous Thrombosis" (PDF). American Venous Forum. Archived from the original (PDF) on September 27, 2016. Retrieved December 24, 2016.
- ^ a b c d e f g h i j k l m n o p q r s t u Hoffman B (2012). Williams gynecology. New York: McGraw-Hill Medical. pp. 960–968. ISBN 978-0071716727.
- ^ Cameron AC, McCallum L, Gardiner T, Darroch C, Walters MR, Oldroyd KG (November 2015). "Impact of treatment algorithms on the prescribing of antithrombotic therapy in patients with suspected acute coronary syndrome – a prospective audit". British Journal of Clinical Pharmacology. 80 (5): 1176–1184. doi:10.1111/bcp.12714. PMC 4631190. PMID 26147691.
- ^ "Patients with Venous Thromboembolism ) Registry". RIETE. Retrieved December 20, 2016.
- ^ a b c d e f g h i j k l m n o Moliterno D (2013). Therapeutic advances in thrombosis. Chichester, West Sussex: Wiley-Blackwell. pp. 306–327. ISBN 978-1405196253.
- ^ a b c d e f g h i j Rosdahl C (2012). Textbook of basic nursing. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 789. ISBN 978-1605477725.
- ^ a b c d e f g h "DVT: Myths vs. Facts | American Society of Hematology". Retrieved December 22, 2016.
- ^ a b c d e Drake R (2012). Gray's basic anatomy, with Student Consult. Philadelphia: Elsevier/Churchill Livingstone. pp. 133–205. ISBN 978-1455710782.
- ^ a b c d e f g h i j k l m n o p Copstead L (2013). Pathophysiology. St. Louis, Mo: Elsevier. pp. 320–329. ISBN 978-1455726509.
- ^ a b c d e f g h Lilley, p. 423.
- ^ a b c d e f g h i j k l m n o p q r s t Kee J (2012). Pharmacology : a nursing process approach. St. Louis, MO: Elsevier Saunders. p. 670–677. ISBN 978-1437717112.
- ^ a b c d e f g Abele H (2014). Atlas of gynecologic surgery. Stuttgart: Thieme. ISBN 978-3136507049; Access provided by the University of Pittsburgh
{{cite book}}: CS1 maint: postscript (link) - ^ a b de Bastos M, Stegeman BH, Rosendaal FR, Van Hylckama Vlieg A, Helmerhorst FM, Stijnen T, Dekkers OM (March 2014). "Combined oral contraceptives: venous thrombosis". The Cochrane Database of Systematic Reviews. 2014 (3): CD010813. doi:10.1002/14651858.CD010813.pub2. PMC 10637279. PMID 24590565.
- ^ Swystun LL, Liaw PC (August 2016). "The role of leukocytes in thrombosis". Blood. 128 (6): 753–762. doi:10.1182/blood-2016-05-718114. PMID 27354721.
- ^ a b c d e Modi S, Deisler R, Gozel K, Reicks P, Irwin E, Brunsvold M, et al. (2016). "Wells criteria for DVT is a reliable clinical tool to assess the risk of deep venous thrombosis in trauma patients". World Journal of Emergency Surgery. 11 (1): 24. doi:10.1186/s13017-016-0078-1. PMC 4898382. PMID 27279896.
- ^ a b c d e f g h i j k Markovchick V (2016). Emergency medicine secrets. Philadelphia, PA: Elsevier. pp. 190–95. ISBN 978-0323355162.
- ^ "Deep Vein Thrombosis & Pulmonary Embolism, Chapter 2, Travelers' Health". CDC. Retrieved December 25, 2016. This article incorporates text from this source, which is in the public domain.
- ^ a b Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, Samama CM (February 2012). "Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis 9th ed, American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e227S–e277S. doi:10.1378/chest.11-2297. PMC 3278061. PMID 22315263.
- ^ a b Stewart DW, Freshour JE (January 2013). "Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence". The Annals of Pharmacotherapy. 47 (1): 63–74. doi:10.1345/aph.1R331. PMID 23324504. S2CID 9366072.
- ^ Stemmer R (February 2013). "Compression Bulletin 24" (PDF). Sigvaris. p. 2. Archived from the original (PDF) on June 20, 2015. Retrieved December 21, 2016.
- ^ a b Streiff MB, Lau BD, Hobson DB, Kraus PS, Shermock KM, Shaffer DL, et al. (December 2016). "The Johns Hopkins Venous Thromboembolism Collaborative: Multidisciplinary team approach to achieve perfect prophylaxis". Journal of Hospital Medicine. 11 (Suppl 2): S8–S14. doi:10.1002/jhm.2657. PMID 27925423.
- ^ "The 2015 Healthcare-Associated Venous Thromboembolism Prevention Challenge Champions". CDC. December 7, 2016. Retrieved December 28, 2016. This article incorporates text from this source, which is in the public domain.
- ^ Minami CA, Yang AD, Ju M, Culver E, Seifert K, Kreutzer L, et al. (December 2016). "Evaluation of an institutional project to improve venous thromboembolism prevention". Journal of Hospital Medicine. 11 (Suppl 2): S29–S37. doi:10.1002/jhm.2663. PMID 27925424.
- ^ "Frequently Asked questions". Thrombosis UK. 2015. Retrieved December 29, 2016.
- ^ a b Potter P (2013). Fundamentals of nursing. St. Louis, Mo: Mosby Elsevier. p. 1149. ISBN 978-0323079334.
- ^ a b Kahn, Susan R.; Morrison, David R.; Diendéré, Gisèle; Piché, Alexandre; Filion, Kristian B.; Klil-Drori, Adi J.; Douketis, James D.; Emed, Jessica; Roussin, André; Tagalakis, Vicky; Morris, Martin (April 24, 2018). "Interventions for implementation of thromboprophylaxis in hospitalized patients at risk for venous thromboembolism". The Cochrane Database of Systematic Reviews. 2018 (4): CD008201. doi:10.1002/14651858.CD008201.pub3. ISSN 1469-493X. PMC 6747554. PMID 29687454.
- ^ "Evidence Summary: Bleeding Risks With Aspirin Use: Aspirin Use to Prevent Cardiovascular Disease and Colorectal Cancer: Preventive Medication". US Preventive Services Task Force. April 2016. Retrieved December 29, 2016.
- ^ a b c d e f g h i j k l m n o p q Henry N (2016). RN pharmacology for nursing : review module. Overland Park, KS: Assessment Technologies Institute. pp. 191–98. ISBN 978-1565335738.
- ^ "Final Update Summary: Aspirin Use to Prevent Cardiovascular Disease and Colorectal Cancer: Preventive Medication". US Preventive Services Task Force. April 2016. Retrieved December 29, 2016.
- ^ "Talk with Your Doctor about Taking Aspirin Every Day". US Preventive Services Task Force. April 2016. Retrieved December 29, 2016.
- ^ "Dipyridamole" at Dorland's Medical Dictionary
- ^ a b c "Recommended Use of Aspirin and Other Antiplatelet Medications Among Adults, National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, United States, 2005–2008". Centers for Disease Control and Prevention. June 15, 2012. Retrieved December 29, 2016.
- ^ "Dipyridamole Monograph for Professionals". Retrieved December 29, 2016.
- ^ Zareba P, Wu C, Agzarian J, Rodriguez D, Kearon C (August 2014). "Meta-analysis of randomized trials comparing combined compression and anticoagulation with either modality alone for prevention of venous thromboembolism after surgery". The British Journal of Surgery. 101 (9): 1053–62. doi:10.1002/bjs.9527. PMID 24916118. S2CID 37373926.
- ^ Kakkar VV, Cohen AT, Mohamed MS (1996). "Patients at risk of venous thromboembolism—clinical results with reviparin". Thrombosis Research. 81 (2 Suppl): S39-45. doi:10.1016/0049-3848(95)00228-6. PMID 8822126.
- ^ Lassen MR, Backs S, Borris LC, Kaltoft-Sørenson M, Coff-Ganes H, Jeppesen E (1999). "Deep-vein thrombosis prophylaxis in orthopedic surgery: hip surgery". Seminars in Thrombosis and Hemostasis. 25 (Suppl 3): 79–82. PMID 10549720.
- ^ Bruner, p. 875–6.
- ^ Garcia DA, Baglin TP, Weitz JI, Samama MM (February 2012). "Parenteral anticoagulants: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e24S–e43S. doi:10.1378/chest.11-2291. PMC 3278070. PMID 22315264.
- ^ Azhar RA, Bochner B, Catto J, Goh AC, Kelly J, Patel HD, et al. (July 2016). "Enhanced Recovery after Urological Surgery: A Contemporary Systematic Review of Outcomes, Key Elements, and Research Needs". European Urology. 70 (1): 176–187. doi:10.1016/j.eururo.2016.02.051. PMC 5514421. PMID 26970912.
- ^ "Computerized Registry of Patients with Veneous Thromboembolism — RIETE Registry". S & H Medical Science Service. Retrieved February 13, 2016.