Disease-modifying antirheumatic drugs (DMARDs) comprise a category of otherwise unrelated disease-modifying drugs defined by their use in rheumatoid arthritis to slow down disease progression.[1][2] The term is often used in contrast to nonsteroidal anti-inflammatory drugs (which refers to agents that treat the inflammation, but not the underlying cause) and steroids (which blunt the immune response but are insufficient to slow down the progression of the disease).
The term "antirheumatic" can be used in similar contexts, but without making a claim about an effect on the disease course.[3] Other terms that have historically been used to refer to the same group of drugs are "remission-inducing drugs" (RIDs) and "slow-acting antirheumatic drugs" (SAARDs).[4]
Terminology
editAlthough the use of the term DMARDs was first propagated in rheumatoid arthritis (hence their name), the term has come to pertain to many other diseases, such as Crohn's disease, lupus erythematosus, Sjögren syndrome, immune thrombocytopenic purpura, myasthenia gravis, sarcoidosis, and various others. [citation needed]
The term was originally introduced to indicate a drug that reduces evidence of processes thought to underlie the disease, such as a raised erythrocyte sedimentation rate, reduced haemoglobin level, raised rheumatoid factor level, and more recently, a raised C-reactive protein level.[citation needed] More recently, the term has been used to indicate a drug that reduces the rate of damage to bone and cartilage.[citation needed] DMARDs can be further subdivided into traditional small molecular mass drugs synthesised chemically and newer "biological" agents produced through genetic engineering.
Some DMARDs (e.g. the purine synthesis inhibitors) are mild chemotherapeutics, but use a side effect of chemotherapy—immunosuppression—as their main therapeutical benefit.[citation needed]
Subdivision
editDMARDs have been classified as:[5]
- synthetic (sDMARD)
- conventional synthetic and targeted synthetic DMARDs (csDMARDs and tsDMARDs, respectively)
- csDMARDs are the traditional drugs (such as methotrexate, sulfasalazine, leflunomide, hydroxychloroquine, gold salts)
- tsDMARDs are drugs that were developed to target a particular molecular structure
- conventional synthetic and targeted synthetic DMARDs (csDMARDs and tsDMARDs, respectively)
- biological (bDMARD) can be further separated into original and biosimilar DMARDs (boDMARDs and bsDMARDs)
- bsDMARDs are those that have the same primary, secondary, and tertiary structure as an original (boDMARD) and possess similar efficacy and safety as the original protein
Members
edit| Drug | Mechanism | Type |
|---|---|---|
| abatacept | T-cell costimulatory signal inhibitor | bDMARD |
| adalimumab | TNF inhibitor | bDMARD |
| anakinra | IL-1 receptor antagonist | bDMARD |
| apremilast | phosphodiesterase 4 (PDE4) inhibitor | tsDMARD |
| azathioprine | Purine synthesis inhibitor | unknown |
| baricitinib | JAK1 and JAK2 inhibitor | tsDMARD |
| certolizumab pegol | TNF inhibitor | bDMARD |
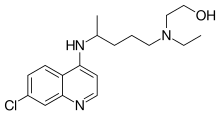
| chloroquine (anti-malarial) | Suppression of IL-1, induce apoptosis of inflammatory cells and decrease chemotaxis | unknown |
| ciclosporin (Cyclosporin A) | calcineurin inhibitor | unknown |
| D-penicillamine (seldom used today) | Reducing numbers of T-lymphocytes etc. | unknown |
| etanercept | decoy TNF receptor | bDMARD |
| filgotinib | Janus kinase (JAK) inhibitor | tsDMARD |
| golimumab | TNF inhibitor | bDMARD |
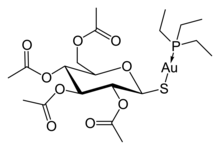
| gold salts (sodium aurothiomalate, auranofin) (seldom used today) | unknown | csDMARD |
| hydroxychloroquine (anti-malarial) | TNF-alpha, induce apoptosis of inflammatory cells and decrease chemotaxis | csDMARD |
| infliximab | TNF inhibitor | bDMARD |
| leflunomide | Pyrimidine synthesis inhibitor | csDMARD |
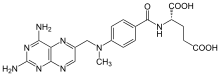
| methotrexate (MTX) | Purine metabolism inhibitor | csDMARD |
| minocycline | 5-LO inhibitor | unknown |
| rituximab | chimeric monoclonal antibody against CD20 on B-cell surface | bDMARD |
| sarilumab | IL-6 receptor antagonist | bDMARD |
| secukinumab | IL-17 inhibitor | bDMARD |
| sulfasalazine (SSZ) | Suppression of IL-1 & TNF-alpha, induce apoptosis of inflammatory cells and increase chemotactic factors | csDMARD |
| tocilizumab | IL-6 receptor antagonist | bDMARD |
| tofacitinib | Janus kinase (JAK) inhibitor | tsDMARD |
| upadacitinib | Janus kinase (JAK) inhibitor | tsDMARD |
| ustekinumab | IL-12 and IL-23 inhibitor | bDMARD |
Although these agents operate by different mechanisms, many of them can have similar impacts upon the course of a condition.[6] Some of the drugs can be used in combination.[7] A common triple therapy for rheumatoid arthritis is methotrexate, sulfasalazine, and hydroxychloroquine.[8]
Alternatives
editWhen treatment with DMARDs fails, cyclophosphamide or steroid pulse therapy is often used to stabilise uncontrolled autoimmune disease. Some severe autoimmune diseases are being treated with bone marrow transplants in clinical trials, usually after cyclophosphamide therapy has failed. Furthermore, should DMARDs fail, tocilizumab can be used for tumor necrosis factor (TNF) inhibitor treatments in NICE guidance.[9]
Combinations of DMARDs are often used, because each drug in the combination can be used in a smaller dose than if it were given alone, thus reducing the risk of side effects.[citation needed]
Many patients receive an NSAID and at least one DMARD, sometimes with low-dose oral glucocorticoids. If disease remission is observed, regular NSAIDs or glucocorticoid treatment may no longer be needed. DMARDs help control arthritis, but do not cure the disease. For that reason, if remission or optimal control is achieved with a DMARD, it is often continued as a maintenance dosage. Discontinuing a DMARD may reactivate disease or cause a "rebound flare", with no assurance that disease control will be re-established upon resumption of the medication.[citation needed]
References
edit- ^ "disease-modifying antirheumatic drug" at Dorland's Medical Dictionary
- ^ "Disease modifying antirheumatic drugs (DMARDs)". Archived from the original on 2009-04-26. Retrieved 2008-10-22.
- ^ "antirheumatic" at Dorland's Medical Dictionary
- ^ Buer, Jonas Kure (2015). "A history of the term "DMARD"". Inflammopharmacology. 23 (4): 163–71. doi:10.1007/s10787-015-0232-5. PMC 4508364. PMID 26002695.
- ^ Smolen JS, van der Heijde D, Machold KP, Aletaha D, Landewé R. Proposal for a new nomenclature of disease-modifying antirheumatic drugs. Ann Rheum Dis. 2014 Jan;73(1):3–5. doi:10.1136/annrheumdis-2013-204317.
- ^ Nandi P, Kingsley GH, Scott DL (May 2008). "Disease-modifying antirheumatic drugs other than methotrexate in rheumatoid arthritis and seronegative arthritis". Current Opinion in Rheumatology. 20 (3): 251–56. doi:10.1097/BOR.0b013e3282fb7caa. PMID 18388514. S2CID 7278909.
- ^ Capell HA, Madhok R, Porter DR, et al. (February 2007). "Combination therapy with sulfasalazine and methotrexate is more effective than either drug alone in patients with rheumatoid arthritis with a suboptimal response to sulfasalazine: results from the double-blind placebo-controlled MASCOT study". Annals of the Rheumatic Diseases. 66 (2): 235–41. doi:10.1136/ard.2006.057133. PMC 1798490. PMID 16926184.
- ^ Donahue, Katrina E.; Gartlehner, Gerald; Schulman, Elizabeth R.; Jonas, Beth; Coker-Schwimmer, Emmanuel; Patel, Sheila V.; Weber, Rachel Palmieri; Lohr, Kathleen N.; Bann, Carla (2018-07-16). Drug Therapy for Early Rheumatoid Arthritis: A Systematic Review Update. Effective Health Care Program (Report). Agency for Healthcare Research and Quality. doi:10.23970/ahrqepccer211. Archived from the original on Oct 19, 2020.
- ^ "Tocilizumab for the Treatment of Rheumatoid Arthritis (TA247)". MIMS. February 2012. Archived from the original on Dec 28, 2014. Retrieved 11 April 2018.