Rift Valley fever (RVF) is a viral disease of humans and livestock that can cause mild to severe symptoms. The mild symptoms may include: fever, muscle pains, and headaches which often last for up to a week. The severe symptoms may include: loss of sight beginning three weeks after the infection, infections of the brain causing severe headaches and confusion, and bleeding together with liver problems which may occur within the first few days. Those who have bleeding have a chance of death as high as 50%.
| Rift Valley fever | |
|---|---|
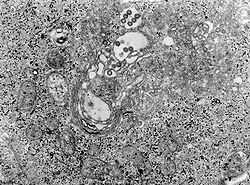 | |
| TEM micrograph of tissue infected with Rift Valley fever virus | |
| Specialty | Infectious diseases, veterinary medicine |
| Symptoms | Fever, muscle pains, headaches |
| Complications | Loss of sight, confusion, bleeding, liver problems |
| Duration | Up to a week |
| Causes | Phlebovirus spread by an infected animal or mosquito |
| Diagnostic method | Finding antibodies or the virus in the blood> |
| Prevention | Vaccinating animals against the disease, decreasing mosquito bites |
| Treatment | Supportive care[1] |
| Frequency | Outbreaks in Africa and Arabia |
The disease is caused by the RVF virus. It is spread by either touching infected animal blood, breathing in the air around an infected animal being butchered, drinking raw milk from an infected animal, or the bite of infected mosquitoes. Animals such as cows, sheep, goats, and camels may be affected. In these animals it is spread mostly by mosquitoes.[1] It does not appear that one person can infect another person. The disease is diagnosed by finding antibodies against the virus or the virus itself in the blood. Prevention of the disease in humans is accomplished by vaccinating animals against the disease. This must be done before an outbreak occurs because if it is done during an outbreak it may worsen the situation. Stopping the movement of animals during an outbreak may also be useful, as may decreasing mosquito numbers and avoiding their bites. There is a human vaccine; however, as of 2010 it is not widely available. There is no specific treatment and medical efforts are supportive.
Outbreaks of the disease have only occurred in Africa and Arabia. Outbreaks usually occur during periods of increased rain which increase the number of mosquitoes. The disease was first reported among livestock in Rift Valley of Kenya in the early 1900s,[2] and the virus was first isolated in 1931.[1]
Signs and symptoms
editIn humans, the virus can cause several syndromes. Usually, they have either no symptoms or only a mild illness with fever, headache, muscle pains, and liver abnormalities. In a small percentage of cases (< 2%), the illness can progress to hemorrhagic fever syndrome, meningoencephalitis (inflammation of the brain and tissues lining the brain), or affect the eye. Patients who become ill usually experience fever, generalised weakness, back pain, dizziness, and weight loss at the onset of the illness. Typically, people recover within two to seven days after onset. About 1% of people with the disease die of it. In livestock, the fatality level is significantly higher. Pregnant livestock infected with RVF abort virtually 100% of foetuses. An epizootic (animal disease epidemic) of RVF is usually first indicated by a wave of unexplained abortions.[citation needed]
Other signs in livestock include vomiting and diarrhea, respiratory disease, fever, lethargy, anorexia and sudden death in young animals.[3]
Cause
editVirology
edit| Rift Valley fever phlebovirus | |
|---|---|
| Phlebovirus virion and genome | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Ellioviricetes |
| Order: | Bunyavirales |
| Family: | Phenuiviridae |
| Genus: | Phlebovirus |
| Species: | Rift Valley fever phlebovirus
|
The virus belongs to the Bunyavirales order. This is an order of enveloped negative single stranded RNA viruses. All Bunyaviruses have an outer lipid envelope with two glycoproteins—G(N) and G(C)—required for cell entry. They deliver their genome into the host-cell cytoplasm by fusing their envelope with an endosomal membrane.[citation needed]
The virus' G(C) protein has a class II membrane fusion protein architecture similar to that found in flaviviruses and alphaviruses.[4] This structural similarity suggests that there may be a common origin for these viral families.[citation needed]
The virus' 11.5 kb tripartite genome is composed of single-stranded RNA. As a Phlebovirus, it has an ambisense genome. Its L and M segments are negative-sense, but its S segment is ambisense.[5] These three genome segments code for six major proteins: L protein (viral polymerase), the two glycoproteins G(N) and G(C), the nucleocapsid N protein, and the nonstructural NSs and NSm proteins.[6]
Transmission
editThe virus is transmitted through mosquito vectors, as well as through contact with the tissue of infected animals. Two species—Culex tritaeniorhynchus and Aedes vexans—are known to transmit the virus.[7] Other potential vectors include Aedes caspius, Aedes mcintosh, Aedes ochraceus, Culex pipiens, Culex antennatus, Culex perexiguus, Culex zombaensis and Culex quinquefasciatus.[8][9][10] Contact with infected tissue is considered to be the main source of human infections.[11] The virus has been isolated from two bat species: the Peter's epauletted fruit bat (Micropteropus pusillus) and the aba roundleaf bat (Hipposideros abae), which are believed to be reservoirs for the virus.[12]
Pathogenesis
editAlthough many components of the RVFV's RNA play an important role in the virus' pathology, the nonstructural protein encoded on the S segment (NSs) is the only component that has been found to directly affect the host. NSs is hostile and combative against the host interferon (IFNs) antiviral response.[13] IFNs are essential in order for the immune system to fight off viral infections in a host.[14] This inhibitory mechanism is believed to be due to a number of reasons, the first being, competitive inhibition of the formation of the transcription factor.[13] On this transcription factor, NSs interacts with and binds to a subunit that is needed for RNA polymerase I and II.[13][15] This interaction cause competitive inhibition with another transcription factor component and prevents the assembly process of the transcription factor complex, which results in the suppression of the host antiviral response.[13][15] Transcription suppression is believed to be another mechanism of this inhibitory process.[13] This occurs when an area of NSs interacts with and binds to the host's protein, SAP30 and forms a complex.[13][15] This complex causes histone acetylation to regress, which is needed for transcriptional activation of the IFN promoter.[15] This causes IFN expression to be obstructed. Lastly, NSs has also been known to affect regular activity of double-stranded RNA-dependent protein kinase R. This protein is involved in cellular antiviral responses in the host. When RVFV is able to enter the host's DNA, NSs forms a filamentous structure in the nucleus. This allows the virus to interact with specific areas of the host's DNA that relates to segregation defects and induction of chromosome continuity. This increases host infectivity and decreases the host's antiviral response.[13]
Diagnosis
editDiagnosis relies on viral isolation from tissues, or serological testing with an ELISA.[3] Other methods of diagnosis include Nucleic Acid Testing (NAT), cell culture, and IgM antibody assays.[16] As of September 2016, the Kenya Medical Research Institute (KEMRI) has developed a product called Immunoline, designed to diagnose the disease in humans much faster than in previous methods.[17]
Prevention
editA person's chances of becoming infected can be reduced by taking measures to decrease contact with blood, body fluids, or tissues of infected animals and protection against mosquitoes and other bloodsucking insects. Use of mosquito repellents and bed nets are two effective methods. For persons working with animals in RVF-endemic areas, wearing protective equipment to avoid any exposure to blood or tissues of animals that may potentially be infected is an important protective measure.[18] Potentially, establishing environmental monitoring and case surveillance systems may aid in the prediction and control of future RVF outbreaks.[18]
No vaccines are currently available for humans. While a vaccines have been developed for humans, it has only been used experimentally for scientific personnel in high-risk environments.[1] Trials of a number of vaccines, such as NDBR-103 and TSI-GSD 200, are ongoing.[19] Different types of vaccines for veterinary use are available. The killed vaccines are not practical in routine animal field vaccination because of the need of multiple injections. Live vaccines require a single injection but are known to cause birth defects and abortions in sheep and induce only low-level protection in cattle. The live-attenuated vaccine, MP-12, has demonstrated promising results in laboratory trials in domesticated animals, but more research is needed before the vaccine can be used in the field. The live-attenuated clone 13 vaccine was recently registered and used in South Africa. Alternative vaccines using molecular recombinant constructs are in development and show promising results.[18]
A vaccine has been conditionally approved for use in animals in the US.[20] It has been shown that knockout of the NSs and NSm nonstructural proteins of this virus produces an effective vaccine in sheep as well.[21]
Epidemiology
editRVF outbreaks occur across sub-Saharan Africa, with outbreaks occurring elsewhere infrequently. Outbreaks of this disease usually correspond with the warm phases of the EI Niño/Southern Oscillation. During this time there is an increase in rainfall, flooding and greenness of vegetation index, which leads to an increase in mosquito vectors.[22] RVFV can be transmitted vertically in mosquitos, meaning that the virus can be passed from the mother to her offspring. During dry conditions, the virus can remain viable for a number of years in the egg. Mosquitos lay their eggs in water, where they eventually hatch. As water is essential for mosquito eggs to hatch, rainfall and flooding cause an increase in the mosquito population and an increased potential for the virus.[23]
The first documented outbreak was identified in Kenya in 1931, in sheep, cattle and humans;[24] another severe outbreak in the country in 1950–1951 involved 100,000 deaths in livestock and an unrecorded number of humans with fever.[25] An outbreak occurred in South Africa in 1974–1976, with more than 500,000 infected animals and the first deaths in humans.[26][27] In Egypt in 1977–78, an estimated 200,000 people were infected and there were at least 594 deaths.[28][29] In Kenya in 1998, the virus killed more than 400 people.[citation needed] Since then, there have been outbreaks in Saudi Arabia and Yemen (2000),[citation needed] East Africa (2006–2007),[30] Sudan (2007),[31] South Africa (2010),[32][33] Uganda (2016),[34] Kenya (2018),[35] and Mayotte (2018–2019).[36] 2020–2021 in Kenya,[37] in 2022 an outbreak is ongoing in Burundi.
Biological weapon
editRift Valley fever was one of more than a dozen agents that the United States researched as potential biological weapons before the nation suspended its biological weapons program in 1969.[38][39]
Research
editThe disease is one of several identified by WHO as a likely cause of a future epidemic in a new plan developed after the Ebola epidemic for urgent research and development toward new diagnostic tests, vaccines and medicines.[40][41]
See also
editReferences
edit- ^ a b c d "Rift Valley fever". Fact sheet N°207. World Health Organization. May 2010. Archived from the original on 15 April 2014. Retrieved 21 March 2014.
- ^ Palmer SR (2011). Oxford textbook of zoonoses : biology, clinical practice, and public health control (2nd ed.). Oxford u.a.: Oxford Univ. Press. p. 423. ISBN 9780198570028. Archived from the original on 2017-09-08.
- ^ a b Rift Valley Fever Archived 2012-05-08 at the Wayback Machine reviewed and published by WikiVet, accessed 12 October 2011.
- ^ Dessau M, Modis Y (January 2013). "Crystal structure of glycoprotein C from Rift Valley fever virus". Proceedings of the National Academy of Sciences of the United States of America. 110 (5): 1696–701. Bibcode:2013PNAS..110.1696D. doi:10.1073/pnas.1217780110. PMC 3562824. PMID 23319635.
- ^ "ViralZone: Phlebovirus". viralzone.expasy.org. Archived from the original on 2016-10-03. Retrieved 2016-09-14.
- ^ Bird BH, Khristova ML, Rollin PE, Ksiazek TG, Nichol ST (2007-03-15). "Complete Genome Analysis of 33 Ecologically and Biologically Diverse Rift Valley Fever Virus Strains Reveals Widespread Virus Movement and Low Genetic Diversity due to Recent Common Ancestry". Journal of Virology. 81 (6): 2805–2816. doi:10.1128/JVI.02095-06. ISSN 0022-538X. PMC 1865992. PMID 17192303.
- ^ Jupp PG, Kemp A, Grobbelaar A, Lema P, Burt FJ, Alahmed AM, Al Mujalli D, Al Khamees M, Swanepoel R (September 2002). "The 2000 epidemic of Rift Valley fever in Saudi Arabia: mosquito vector studies". Medical and Veterinary Entomology. 16 (3): 245–52. doi:10.1046/j.1365-2915.2002.00371.x. PMID 12243225.
- ^ Turell MJ, Presley SM, Gad AM, Cope SE, Dohm DJ, Morrill JC, Arthur RR (February 1996). "Vector competence of Egyptian mosquitoes for Rift Valley fever virus". The American Journal of Tropical Medicine and Hygiene. 54 (2): 136–39. doi:10.4269/ajtmh.1996.54.136. PMID 8619436.
- ^ Turell MJ, Lee JS, Richardson JH, Sang RC, Kioko EN, Agawo MO, Pecor J, O'Guinn ML (December 2007). "Vector competence of Kenyan Culex zombaensis and Culex quinquefasciatus mosquitoes for Rift Valley fever virus". Journal of the American Mosquito Control Association. 23 (4): 378–82. doi:10.2987/5645.1. PMID 18240513. S2CID 36591701.
- ^ Fontenille D, Traore-Lamizana M, Diallo M, Thonnon J, Digoutte JP, Zeller HG (1998). "New vectors of Rift Valley fever in West Africa". Emerging Infectious Diseases. 4 (2): 289–93. doi:10.3201/eid0402.980218. PMC 2640145. PMID 9621201.
- ^ Swanepoel R, Coetzer JA (2004). "Rift Valley fever". In Coetzer JA, Tustin RC (eds.). Infectious diseases of livestock (2nd ed.). Cape Town: Oxford University Press Southern Africa. pp. 1037–70. ISBN 978-0195761702.
- ^ Boiro I, Konstaninov OK, Numerov AD (1987). "[Isolation of Rift Valley fever virus from bats in the Republic of Guinea]". Bulletin de la Société de Pathologie Exotique et de Ses Filiales (in French). 80 (1): 62–67. PMID 3607999.
- ^ a b c d e f g Boshra H, Lorenzo G, Busquets N, Brun A (July 2011). "Rift valley fever: recent insights into pathogenesis and prevention". Journal of Virology. 85 (13): 6098–105. doi:10.1128/JVI.02641-10. PMC 3126526. PMID 21450816.
- ^ Fensterl V, Sen GC (2009-01-01). "Interferons and viral infections". BioFactors. 35 (1): 14–20. doi:10.1002/biof.6. PMID 19319841. S2CID 27209861.
- ^ a b c d Ikegami T, Makino S (May 2011). "The pathogenesis of Rift Valley fever". Viruses. 3 (5): 493–519. doi:10.3390/v3050493. PMC 3111045. PMID 21666766.
- ^ Fields BN, Knipe DM, Howley PM (2013). Fields Virology, 6th Edition. Philadelphia, PA: Wolters Kluwer, Lippincott Williams & Wilkins. p. 441. ISBN 978-1-4511-0563-6.
- ^ "Kemri develops kit for rapid test of viral disease". Archived from the original on 2016-09-06. Retrieved 2016-09-14.
- ^ a b c "Prevention: Rift Valley Fever | CDC". US Centers for Disease Control and Prevention. Retrieved 24 September 2018. This article incorporates text from this source, which is in the public domain.
- ^ Fawzy M, Helmy YA (February 2019). "The One Health Approach is Necessary for the Control of Rift Valley Fever Infections in Egypt: A Comprehensive Review". Viruses. 11 (2): 139. doi:10.3390/v11020139. PMC 6410127. PMID 30736362.
- ^ Ikegami T, Hill TE, Smith JK, Zhang L, Juelich TL, Gong B, Slack OA, Ly HJ, Lokugamage N, Freiberg AN (July 2015). "Rift Valley Fever Virus MP-12 Vaccine Is Fully Attenuated by a Combination of Partial Attenuations in the S, M, and L Segments". Journal of Virology. 89 (14): 7262–76. doi:10.1128/JVI.00135-15. PMC 4473576. PMID 25948740.
- ^ Bird BH, Maartens LH, Campbell S, Erasmus BJ, Erickson BR, Dodd KA, Spiropoulou CF, Cannon D, Drew CP, Knust B, McElroy AK, Khristova ML, Albariño CG, Nichol ST (December 2011). "Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep". Journal of Virology. 85 (24): 12901–09. doi:10.1128/JVI.06046-11. PMC 3233145. PMID 21976656.
- ^ Nanyingi MO, Munyua P, Kiama SG, Muchemi GM, Thumbi SM, Bitek AO, Bett B, Muriithi RM, Njenga MK (2015-07-31). "A systematic review of Rift Valley Fever epidemiology 1931–2014". Infection Ecology & Epidemiology. 5 (1): 28024. Bibcode:2015InfEE...528024N. doi:10.3402/iee.v5.28024. PMC 4522434. PMID 26234531. Archived from the original on 2016-12-02.
- ^ "Rift Valley Fever | CDC". www.cdc.gov. Archived from the original on 2016-12-04. Retrieved 2016-12-01.
- ^ Daubney R, Hudson JR, Garnham PC (1931). "Enzootic hepatitis or rift valley fever. An undescribed virus disease of sheep cattle and man from east africa". The Journal of Pathology and Bacteriology. 34 (4): 545–79. doi:10.1002/path.1700340418.
- ^ Murithi RM, Munyua P, Ithondeka PM, Macharia JM, Hightower A, Luman ET, Breiman RF, Njenga MK (March 2011). "Rift Valley fever in Kenya: history of epizootics and identification of vulnerable districts". Epidemiology and Infection. 139 (3): 372–80. doi:10.1017/S0950268810001020. PMID 20478084. S2CID 41617078.
- ^ McMillen CM, Hartman AL (2018). "Rift Valley fever in animals and humans: Current perspectives". Antiviral Research. 156: 29–37. doi:10.1016/j.antiviral.2018.05.009. PMC 10316118. PMID 29857007. S2CID 46918400.
- ^ van Velden DJ, Meyer JD, Olivier J, Gear JH, McIntosh B (1977-06-11). "Rift Valley fever affecting humans in South Africa: a clinicopathological study". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 51 (24): 867–71. PMID 561445.
- ^ Arzt J, White WR, Thomsen BV, Brown CC (January 2010). "Agricultural diseases on the move early in the third millennium". Veterinary Pathology. 47 (1): 15–27. doi:10.1177/0300985809354350. PMID 20080480. S2CID 31753926.
- ^ Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ (April 2009). "Rift Valley fever virus". Journal of the American Veterinary Medical Association. 234 (7): 883–93. doi:10.2460/javma.234.7.883. PMID 19335238. S2CID 16239209.
- ^ "At least 75 people die of Rift Valley Fever in Kenya". International Herald Tribune. 7 January 2007. Archived from the original on 9 January 2007.
- ^ "Deadly fever spreads Kenya Panic". BBC. 26 January 2007. Archived from the original on 1 May 2008.
- ^ ProMED-mail Archived 2011-07-28 at the Wayback Machine. ProMED-mail. Retrieved on 2014-05-12.
- ^ "Rift Valley fever in South Africa". WHO. Archived from the original on 2010-04-12.
- ^ "Outbreak Summaries | Rift Valley Fever | CDC". 2019-02-15.
- ^ "Rift Valley fever – Kenya". WHO. 18 June 2018. Archived from the original on June 23, 2018. Retrieved 1 July 2018.
- ^ "Rift Valley Fever – Mayotte (France)". WHO. 13 May 2019. Archived from the original on July 1, 2019. Retrieved 15 May 2019.
- ^ "Rift Valley fever – Kenya". World Health Organization. 12 February 2021. Archived from the original on February 12, 2021. Retrieved 24 February 2021.
- ^ "Chemical and Biological Weapons: Possession and Programs Past and Present", James Martin Center for Nonproliferation Studies, Middlebury College, April 9, 2002, accessed November 14, 2008.
- ^ "Select Agents and Toxins" (PDF). USDA-APHIS and CDC: National Select Agent Registry. 2011-09-19. Archived from the original (PDF) on 2012-02-25.
- ^ Kieny MP. "After Ebola, a Blueprint Emerges to Jump-Start R&D". Scientific American Blog Network. Archived from the original on 20 December 2016. Retrieved 13 December 2016.
- ^ "List of Pathogens". World Health Organization. Archived from the original on 20 December 2016. Retrieved 13 December 2016.
External links
edit- CDC RVF Information Page
- Rift Valley Fever disease card at OIE
- "Rift Valley fever". Fact sheet N°207. World Health Organization. May 2010. Retrieved 21 March 2014.
- "Rift Valley fever virus". NCBI Taxonomy Browser. 11588.