Dabigatran, sold under the brand name Pradaxa among others, is an anticoagulant used to treat and prevent blood clots and to prevent stroke in people with atrial fibrillation.[6][7] Specifically it is used to prevent blood clots following hip or knee replacement and in those with a history of prior clots.[6] It is used as an alternative to warfarin and does not require monitoring by blood tests.[6] In a meta analysis of 7 different studies, there was no benefit of dabigatran over warfarin in preventing ischemic stroke; however, dabigatran were associated with a lower hazard for intracranial bleeding compared with warfarin, but also had a higher risk of gastrointestinal bleeding relative to warfarin.[8] It is taken by mouth.[6]
 | |
| Clinical data | |
|---|---|
| Trade names | Pradaxa, Pradax, Prazaxa, others |
| Other names | BIBR-953, BIBR-1048 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a610024 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Direct thrombin inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 3–7%[6] |
| Protein binding | 35%[6] |
| Elimination half-life | 12–17 hours[6] |
| Identifiers | |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI |
|
| ChEMBL |
|
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
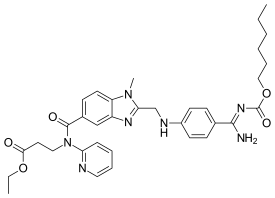
| Formula | C25H25N7O3 |
| Molar mass | 471.521 g·mol−1 |
| 3D model (JSmol) |
|
| |
| |
| | |
Common side effects include bleeding and gastritis.[6] Other side effects may include bleeding around the spine and allergic reactions such as anaphylaxis.[6] In cases of severe bleeding, it can be reversed with the antidote, idarucizumab.[6] Use is not recommended during pregnancy or breastfeeding.[6] Compared to warfarin it has fewer interactions with other medications.[9] It is a direct thrombin inhibitor.[7]
Dabigatran was approved for medical use in the United States in 2010.[6] It is on the World Health Organization's List of Essential Medicines.[10] In 2020, it was the 306th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[11] Dabigatran is available a generic medication.[12][13]
Medical uses
editDabigatran is used to prevent strokes in those with atrial fibrillation not caused by heart valve issues, as well as deep vein thrombosis and pulmonary embolism in persons who have been treated for 5–10 days with parenteral anticoagulant (usually low molecular weight heparin), and to prevent deep vein thrombosis and pulmonary embolism in some circumstances.[4]
It appears to be as effective as warfarin in preventing non-hemorrhagic strokes and embolic events in those with atrial fibrillation not due to valve problems.[14][15][16]
In 2022, an observational meta-analysis study was performed on direct oral anticoagulants for patients with atrial fibrillation. The study found that dabigatran had comparable rates of ischemic stroke or systemic embolism, intracerebral haemorrhage, and all-cause mortality when compared to other anticoagulants like apixaban, edoxaban, and rivaroxaban. Notably, apixaban was associated with a lower risk of gastrointestinal bleeding than dabigatran and the others. This finding was generally steady for patients aged 80 years or older and those with chronic kidney disease.[17]
Contraindications
editDabigatran is contraindicated in patients who have active pathological bleeding, since dabigatran can increase bleeding risk and can also cause serious and potentially life-threatening bleeds.[4] Dabigatran is also contraindicated in patients who have a history of serious hypersensitivity reaction to dabigatran (e.g. anaphylaxis or anaphylactic shock).[4] The use of dabigatran should also be avoided in patients with mechanical prosthetic heart valves due to the increased risk of thromboembolic events (e.g. valve thrombosis, stroke, and myocardial infarction) and major bleeding when compared with warfarin.[4][18][19]
Current FDA guidelines states that patients with mechanical heart valves should not be using dabigatran. The safety and efficacy of Pradaxa (dabigatran) were evaluated in the European RE-ALIGN trial in 2012. RE-ALIGN was terminated early because the Pradaxa treatment group had significantly more thromboembolic events and major bleeding than warfarin and determined to be contraindicated for use in patients with mechanical heart valves.[20] Further studies are needed in order to determine effects of dabigatran on patients with bioprosthetic valves.
Dabigatran is poorly excreted in breastmilk and does not appear to require any limitations to breastfeeding.[21] However, data is limited and further studies are needed.
Adverse effects
editThe most commonly reported side effect of dabigatran is gastrointestinal upset. When compared with people anticoagulated with warfarin, patients taking dabigatran had fewer life-threatening bleeds, fewer minor and major bleeds, including intracranial bleeds, but the rate of gastrointestinal bleeding was significantly higher. Dabigatran capsules contain tartaric acid, which lowers the gastric pH and is required for adequate absorption. The lower pH has previously been associated with dyspepsia; some hypothesize that this plays a role in the increased risk of gastrointestinal bleeding.[22] If a small amount of GI bleeding is diagnosed, the clinicians may consider adding H2 receptor inhibitor (H2RA), proton pump inhibitors (PPIs) and mucosal protective agent. In severe bleeding, measures include discontinuation of dabigatran immediately, and administration of prothrombin complex concentrate, packed red blood cells, fresh frozen plasma, the use of specific reversal agents such as idarucizumab for dabigatran, and emergency endoscopic management.[23]
A small but significantly increased risk of myocardial infarctions (heart attacks) has been noted when combining the safety outcome data from multiple trials.[24][25] However, conflicting evidence from another review suggested that dabigatran might not substantially increase the risk of heart attacks, or if it does, then the associated risk is relatively low.[26]
For patients with moderately reduced kidney function, lower dabigatran doses are recommended due to increased drug exposure and bleeding risk.[27][28][29] Alternative anticoagulants should be considered in severe kidney impairment due to insufficient safety and efficacy data.[28]
Dabigatran intake has also been reported to cause esophageal injury or esophagitis. In a 2016 study by Toya et al., roughly 20% of patients suffered esophageal mucosa damage.[30] It has been theorized that the tartaric-acid core in the drug adheres and damages the esophagus, and then the damaged esophageal mucosa exfoliates after peristalsis.[31] Additionally, patients with limited mobility, reduced salivary secretion, and low water consumption will increase the possibility of contact by dabigatran with the esophageal mucosa.[23]
The Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial showed that impairment of liver function caused by dabigatran occurred in the same frequency as warfarin.[32]
Pharmacology
editMechanism of action
editDabigatran reversibly binds to the active site on the thrombin molecule, preventing thrombin-mediated activation of coagulation factors. Furthermore, dabigatran can inactivate thrombin even when thrombin is fibrin-bound; it reduces thrombin-mediated inhibition of fibrinolysis and, therefore, may enhance fibrinolysis.[33]
Pharmacokinetics
editDabigatran has a half-life of approximately 12–17 h and exerts a maximum anticoagulation effect within 2 hours after ingestion.[34] Fatty foods delay the intestinal absorption of dabigatran, although the bioavailability of the drug is unaffected.[4] Several studies have demonstrated that dabigatran plasma concentrations are reduced when co-administered with proton pump inhibitors, however it is unclear if this reduction is clinically significant.[35][36][37] Dabigatran excretion through P-glycoprotein pumps is slowed in patients taking strong p-glycoprotein pump inhibitors such as quinidine, verapamil, and amiodarone, thus raising plasma levels of dabigatran.[38]
Dabigatran is available as dabigatran etexilate mesilate, formulated as the prodrug dabigatran etexilate.[4][6][38]
History
editDabigatran (then compound BIBR-953) was discovered from a panel of chemicals with similar structure to benzamidine-based thrombin inhibitor α-NAPAP (N-alpha-(2-naphthylsulfonylglycyl)-4-amidinophenylalanine piperidide), which had been known since the 1980s as a powerful inhibitor of various serine proteases, specifically thrombin, but also trypsin. Addition of ethyl ester and hexyloxycarbonyl carbamide hydrophobic side chains led to the orally absorbed prodrug, BIBR 1048 (dabigatran etexilate).[39]
In March 2008, the European Medicines Agency (EMA) granted marketing authorization for Pradaxa for the prevention of thromboembolic disease following hip or knee replacement surgery and for non-valvular atrial fibrillation.[40]
The National Health Service (NHS) in Britain authorized dabigatran for use in preventing blood clots in hip and knee replacement surgery patients. According to a BBC article in 2008, Dabigatran was expected to cost the NHS £4.20 per day, which was similar to several other anticoagulants.[41]
Initially, there was no specific way to reverse the anticoagulant effect of dabigatran in the event of a major bleeding event,[42] unlike for warfarin.[43] Since then, the dabigatran-specific antidote idarucizumab, a humanized monoclonal antibody for intravenous administration, was developed, and received Food and Drug Administration (FDA) approval in 2015.[44]
Pradaxa received a Notice of Compliance (NOC) from Health Canada in June 2008,[45] for the prevention of blood clots in patients who have undergone total hip or total knee replacement surgery. Approval for atrial fibrillation patients at risk of stroke came in October 2010.[46][47]
The U.S. Food and Drug Administration (FDA) approved Pradaxa in October 2010, for prevention of stroke in patients with non-valvular atrial fibrillation.[48][49][50][51] The approval came after an advisory committee recommended the drug for approval in September 2010,[52] although caution is still urged by some outside experts.[53]
In February 2011, the American College of Cardiology Foundation and the American Heart Association added dabigatran to their guidelines for management of non-valvular atrial fibrillation with a class I recommendation.[54]
In May 2014, the FDA reported the results of a large study comparing dabigatran with warfarin in 134,000 Medicare patients. The agency concluded that dabigatran is associated with a lower risk of overall mortality, ischemic stroke, and bleeding in the brain than warfarin. Gastrointestinal bleeding was more common in those treated with dabigatran than in those treated with warfarin. The risk of heart attack was similar between the two drugs. The FDA reiterated its opinion that dabigatran's overall risk/benefit ratio is favorable.[55]
In July 2014, a series of investigations accused the privately held Boehringer Ingelheim pharmaceutical group of withholding critical information about the need for monitoring to protect patients from severe bleeding, particularly in the elderly. Review of internal communications between Boehringer researchers and employees by the FDA and the EMA revealed that Boehringer researchers had found evidence that serum levels of dabigatran vary widely. The BMJ investigation suggested that Boehringer had a financial motive to withhold this concern from regulatory health agencies because the data conflicted with their extensive marketing of dabigatran as an anticoagulant that does not require monitoring.[56][57] In August 2012, Pradaxa claims filed in U.S. federal courts were consolidated into a multi-district litigation in the Southern District of Illinois before Chief Judge David R. Herndon. In May 2014, a $650 million settlement was announced on behalf of approximately 3,900 claimants who were injured by the drug Pradaxa made by Boehringer Ingelheim Pharmaceuticals, Inc. The drug was alleged to cause severe bleeding events and/or hemorrhaging to those who were taking the drug.[58]
References
edit- ^ "Dabigatran (Pradaxa) Use During Pregnancy". Drugs.com. 27 December 2018. Archived from the original on 1 October 2020. Retrieved 16 May 2020.
- ^ "Pradaxa Product information". health-products.canada.ca. 22 October 2009. Retrieved 13 November 2023.
- ^ "Summary of Product Characteristics (SmPC)". (emc). 15 September 2022. Archived from the original on 21 April 2023. Retrieved 13 November 2023.
- ^ a b c d e f g "Pradaxa- dabigatran etexilate mesylate capsule". DailyMed. 6 July 2020. Archived from the original on 28 June 2021. Retrieved 13 November 2020.
- ^ "Pradaxa EPAR". European Medicines Agency. 22 March 2023. Archived from the original on 5 June 2023. Retrieved 13 November 2023.
- ^ a b c d e f g h i j k l m "Dabigatran Etexilate Mesylate Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 27 March 2019. Retrieved 27 March 2019.
- ^ a b British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 135–137. ISBN 9780857113382.
- ^ Romanelli RJ, Nolting L, Dolginsky M, Kym E, Orrico KB (March 2016). "Dabigatran Versus Warfarin for Atrial Fibrillation in Real-World Clinical Practice: A Systematic Review and Meta-Analysis". Circulation: Cardiovascular Quality and Outcomes. 9 (2): 126–134. doi:10.1161/CIRCOUTCOMES.115.002369. PMID 26812933. S2CID 6840541.
- ^ Kiser K (2017). Oral Anticoagulation Therapy: Cases and Clinical Correlation. Springer. p. 11. ISBN 9783319546438.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ "Dabigatran - Drug Usage Statistics". ClinCalc. Archived from the original on 13 November 2022. Retrieved 7 October 2022.
- ^ "Office of Generic Drugs 2020 Annual Report". U.S. Food and Drug Administration (FDA). Archived from the original on 12 February 2021. Retrieved 12 February 2021.
- ^ "Dabigatran Etexilate Accord". European Medicines Agency. 31 May 2023. Retrieved 2 June 2023.
- ^ Gómez-Outes A, Terleira-Fernández AI, Calvo-Rojas G, Suárez-Gea ML, Vargas-Castrillón E (2013). "Dabigatran, Rivaroxaban, or Apixaban versus Warfarin in Patients with Nonvalvular Atrial Fibrillation: A Systematic Review and Meta-Analysis of Subgroups". Thrombosis. 2013: 640723. doi:10.1155/2013/640723. PMC 3885278. PMID 24455237.
- ^ Lowenstern A, Al-Khatib SM, Sharan L, Chatterjee R, Allen LaPointe NM, Shah B, et al. (December 2018). "Interventions for Preventing Thromboembolic Events in Patients With Atrial Fibrillation: A Systematic Review". Annals of Internal Medicine. 169 (11): 774–787. doi:10.7326/M18-1523. PMC 6825839. PMID 30383133.
- ^ Sanders GD, Lowenstern A, Borre E, Chatterjee R, Goode A, Sharan L, et al. (October 2018). Stroke Prevention in Patients With Atrial Fibrillation: A Systematic Review Update. Agency for Healthcare Research and Quality (US) (Report). Rockville (MD). doi:10.23970/ahrqepccer214 (inactive 10 December 2024). PMID 30480925. Report No.: 18-EHC018-EFReport No.: 2018-SR-04. Archived from the original on 29 March 2019. Retrieved 31 May 2023.
{{cite report}}: CS1 maint: DOI inactive as of December 2024 (link) - ^ Lau WC, Torre CO, Man KK, Stewart HM, Seager S, Van Zandt M, et al. (November 2022). "Comparative Effectiveness and Safety Between Apixaban, Dabigatran, Edoxaban, and Rivaroxaban Among Patients With Atrial Fibrillation : A Multinational Population-Based Cohort Study". Annals of Internal Medicine. 175 (11): 1515–1524. doi:10.7326/M22-0511. PMID 36315950. S2CID 253238819.
- ^ "FDA Drug Safety Communication: Pradaxa (dabigatran etexilate mesylate) should not be used in patients with mechanical prosthetic heart valves". U.S. Food and Drug Administration (FDA). Archived from the original on 2 November 2014. Retrieved 29 October 2014.
- ^ Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein AP, Mack MJ, et al. (September 2013). "Dabigatran versus warfarin in patients with mechanical heart valves". The New England Journal of Medicine. 369 (13): 1206–1214. doi:10.1056/NEJMoa1300615. PMID 23991661.
- ^ "FDA Drug Safety Communication: Pradaxa (dabigatran etexilate mesylate) should not be used in patients with mechanical prosthetic heart valves". Center for Drug Evaluation and Research. U.S. Food and Drug Administration. 21 June 2019. Archived from the original on 27 February 2023. Retrieved 27 February 2023.
- ^ "Dabigatran", Drugs and Lactation Database (LactMed®), Bethesda (MD): National Institute of Child Health and Human Development, 2006, PMID 29999803, archived from the original on 2 May 2023, retrieved 27 February 2023
- ^ Blommel ML, Blommel AL (August 2011). "Dabigatran etexilate: A novel oral direct thrombin inhibitor". American Journal of Health-System Pharmacy. 68 (16): 1506–1519. doi:10.2146/ajhp100348. PMID 21817082.
- ^ a b Lin S, Wang Y, Zhang L, Guan W (6 May 2019). "Dabigatran must be used carefully: literature review and recommendations for management of adverse events". Drug Design, Development and Therapy. 13: 1527–1533. doi:10.2147/DDDT.S203112. PMC 6511609. PMID 31190734.
- ^ Uchino K, Hernandez AV (March 2012). "Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials". Archives of Internal Medicine. 172 (5): 397–402. doi:10.1001/archinternmed.2011.1666. PMID 22231617.
- ^ Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. (September 2009). "Dabigatran versus warfarin in patients with atrial fibrillation". The New England Journal of Medicine. 361 (12): 1139–1151. doi:10.1056/NEJMoa0905561. hdl:11343/221723. PMID 19717844.
- ^ Wei AH, Gu ZC, Zhang C, Ding YF, Liu D, Li J, et al. (September 2018). "Increased risk of myocardial infarction with dabigatran etexilate: fact or fiction? A critical meta-analysis of over 580,000 patients from integrating randomized controlled trials and real-world studies". International Journal of Cardiology. 267: 1–7. doi:10.1016/j.ijcard.2018.05.048. PMID 29801762.
- ^ Stangier J, Rathgen K, Stähle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clinical pharmacokinetics. 2010 Apr; 49:259-68.
- ^ a b Hijazi Z, Hohnloser SH, Oldgren J, Andersson U, Connolly SJ, Eikelboom JW, et al. (March 2014). "Efficacy and safety of dabigatran compared with warfarin in relation to baseline renal function in patients with atrial fibrillation: a RE-LY (Randomized Evaluation of Long-term Anticoagulation Therapy) trial analysis". Circulation. 129 (9): 961–970. doi:10.1161/circulationaha.113.003628. PMID 24323795.
- ^ An J, Cheetham TC, Luong T, Lang DT, Lee MS, Reynolds K (July 2023). "Effectiveness and safety of Dabigatran 110 mg versus 150 mg for Stroke Prevention in Patients with Atrial Fibrillation at High Bleeding Risk". Clinical Therapeutics. 45 (7): e151–e158. doi:10.1016/j.clinthera.2023.05.007. PMID 37380555.
- ^ Toya Y, Nakamura S, Tomita K, Matsuda N, Abe K, Abiko Y, et al. (March 2016). "Dabigatran-induced esophagitis: The prevalence and endoscopic characteristics". Journal of Gastroenterology and Hepatology. 31 (3): 610–614. doi:10.1111/jgh.13024. PMID 26102078. S2CID 2601542.
- ^ Bytzer P, Connolly SJ, Yang S, Ezekowitz M, Formella S, Reilly PA, et al. (March 2013). "Analysis of upper gastrointestinal adverse events among patients given dabigatran in the RE-LY trial". Clinical Gastroenterology and Hepatology. 11 (3): 246–252.e5. doi:10.1016/j.cgh.2012.10.021. PMID 23103906.
- ^ Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. (September 2009). "Dabigatran versus warfarin in patients with atrial fibrillation". The New England Journal of Medicine. 361 (12): 1139–1151. doi:10.1056/NEJMoa0905561. hdl:11343/221723. PMID 19717844. S2CID 7425216.
- ^ Comin J, Kallmes DF (March 2012). "Dabigatran (Pradaxa)". AJNR. American Journal of Neuroradiology. 33 (3): 426–428. doi:10.3174/ajnr.A3000. PMC 7966436. PMID 22345499.
- ^ Muñoz-Corcuera M, Ramírez-Martínez-Acitores L, López-Pintor RM, Casañas-Gil E, Hernández-Vallejo G (November 2016). "Dabigatran: A new oral anticoagulant. Guidelines to follow in oral surgery procedures. A systematic review of the literature". Medicina Oral, Patologia Oral y Cirugia Bucal. 21 (6): e679–e688. doi:10.4317/medoral.21202. PMC 5116109. PMID 27694780.
- ^ Stangier J, Eriksson BI, Dahl OE, Ahnfelt L, Nehmiz G, Stähle H, et al. (May 2005). "Pharmacokinetic profile of the oral direct thrombin inhibitor dabigatran etexilate in healthy volunteers and patients undergoing total hip replacement". Journal of Clinical Pharmacology. 45 (5): 555–563. doi:10.1177/0091270005274550. PMID 15831779. S2CID 26441767.
- ^ Kuwayama T, Osanai H, Ajioka M, Tokuda K, Ohashi H, Tobe A, et al. (December 2017). "Influence of proton pump inhibitors on blood dabigatran concentrations in Japanese patients with non-valvular atrial fibrillation". Journal of Arrhythmia. 33 (6): 619–623. doi:10.1016/j.joa.2017.07.013. PMC 5729000. PMID 29255511.
- ^ Bolek T, Samoš M, Stančiaková L, Ivanková J, Škorňová I, Staško J, et al. (May 2019). "The Impact of Proton Pump Inhibition on Dabigatran Levels in Patients With Atrial Fibrillation". American Journal of Therapeutics. 26 (3): e308–e313. doi:10.1097/mjt.0000000000000599. PMID 28452843.
- ^ a b "Pradaxa Summary of Product Characteristics" (2018) Archived 5 July 2019 at the Wayback Machine. European Medicines Agency.
- ^ Hauel NH, Nar H, Priepke H, Ries U, Stassen JM, Wienen W (April 2002). "Structure-based design of novel potent nonpeptide thrombin inhibitors". Journal of Medicinal Chemistry. 45 (9): 1757–1766. doi:10.1021/jm0109513. PMID 11960487.
- ^ "Pradaxa EPAR". European Medicines Agency. Archived from the original on 2 August 2012. Retrieved 30 January 2011.
- ^ "Clot drug 'could save thousands'". BBC News Online. 20 April 2008. Archived from the original on 15 January 2009. Retrieved 21 April 2008.
- ^ van Ryn J, Stangier J, Haertter S, Liesenfeld KH, Wienen W, Feuring M, et al. (June 2010). "Dabigatran etexilate--a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity". Thrombosis and Haemostasis. 103 (6): 1116–1127. doi:10.1160/TH09-11-0758. PMID 20352166. S2CID 37404563.
Although there is no specific antidote to antagonise the anticoagulant effect of dabigatran, due to its short duration of effect drug discontinuation is usually sufficient to reverse any excessive anticoagulant activity.
- ^ Hanley JP (November 2004). "Warfarin reversal". Journal of Clinical Pathology. 57 (11): 1132–1139. doi:10.1136/jcp.2003.008904. PMC 1770479. PMID 15509671.
- ^ Syed YY (August 2016). "Idarucizumab: A Review as a Reversal Agent for Dabigatran". American Journal of Cardiovascular Drugs. 16 (4): 297–304. doi:10.1007/s40256-016-0181-4. PMID 27388764. S2CID 11596083.
- ^ "Summary Basis of Decision (SBD): Pradax" Archived 14 July 2016 at the Wayback Machine Health Canada. 6 November 2008.
- ^ Kirkey S (29 October 2010). "Approval of new drug heralds 'momentous' advance in stroke prevention". Montreal Gazette. Archived from the original on 16 June 2011. Retrieved 29 October 2010.
- ^ "Pradax (Dabigatran Etexilate) Gains Approval In Canada For Stroke Prevention In Atrial Fibrillation" Archived 24 April 2011 at the Wayback Machine Medical News Today. 28 October 2010.
- ^ Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. (September 2009). "Dabigatran versus warfarin in patients with atrial fibrillation". The New England Journal of Medicine. 361 (12): 1139–1151. doi:10.1056/NEJMoa0905561. hdl:11343/221723. PMID 19717844. S2CID 7425216.
- ^ Turpie AG (January 2008). "New oral anticoagulants in atrial fibrillation". European Heart Journal. 29 (2): 155–165. doi:10.1093/eurheartj/ehm575. PMID 18096568.
- ^ "Boehringer wins first US OK in blood-thinner race". Reuters. 19 October 2010. Archived from the original on 4 May 2016. Retrieved 20 October 2010.
- ^ "FDA approves Pradaxa to prevent stroke in people with atrial fibrillation" (Press release). U.S. Food and Drug Administration (FDA). 19 October 2010. Archived from the original on 20 October 2010.
- ^ Shirley S. Wang (20 September 2010). "New Blood-Thinner Recommended by FDA Panel". The Wall Street Journal. Archived from the original on 24 April 2016. Retrieved 20 October 2010.
- ^ Merli G, Spyropoulos AC, Caprini JA (August 2009). "Use of emerging oral anticoagulants in clinical practice: translating results from clinical trials to orthopedic and general surgical patient populations". Annals of Surgery. 250 (2): 219–228. doi:10.1097/SLA.0b013e3181ae6dbe. PMID 19638915. S2CID 44917732.
- ^ Wann LS, Curtis AB, Ellenbogen KA, Estes NA, Ezekowitz MD, Jackman WM, et al. (March 2011). "2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on Dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines". Circulation. 123 (10): 1144–1150. doi:10.1161/CIR.0b013e31820f14c0. PMID 21321155.
- ^ "FDA Drug Safety Communication: FDA study of Medicare patients finds risks lower for stroke and death but higher for gastrointestinal bleeding with Pradaxa (dabigatran) compared to warfarin". U.S. Food and Drug Administration (FDA). 21 June 2019. Archived from the original on 11 November 2020. Retrieved 13 November 2020.
- ^ Cohen D (July 2014). "Dabigatran: how the drug company withheld important analyses". BMJ. 349: g4670. doi:10.1136/bmj.g4670. PMID 25055829.
- ^ Moore TJ, Cohen MR, Mattison DR (July 2014). "Dabigatran, bleeding, and the regulators". BMJ. 349: g4517. doi:10.1136/bmj.g4517. PMID 25056265. S2CID 29090410.
- ^ Thomas K (28 May 2014). "$650 Million to Settle Blood Thinner Lawsuits". The New York Times. Archived from the original on 11 June 2021. Retrieved 26 November 2020.